Abstract
Summary
During the first year of Prospective Observational Scientific Study Investigating Bone Loss Experience (POSSIBE US™), many women transitioned (i.e., discontinued or switched) from their baseline osteoporosis medication. Participants not on stable therapy at entry, with side effects, and with poor physical status were at higher risk of transitioning. Understanding factors associated with persistence may lead to improved outcomes.
Introduction
Postmenopausal osteoporosis (PMO) medication use patterns may differ by treatment history and drug class. We describe these patterns among patients in primary care settings using patient-reported data.
Methods
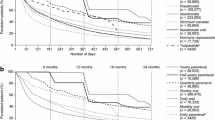
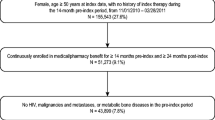
Data from 3,006 participants of the POSSIBLE US™ were used to estimate the probability of a baseline PMO medication transition (i.e., discontinuation or switch) and hazard ratios (HRs) for predictors of these transitions.
Results
One year after study entry, the probability of persisting with a baseline medication was 66% (95% CI: 64–68%). After adjusting for age and osteoporosis diagnosis, factors at entry independently associated with a higher risk of baseline medication transition were treatment status cohort, side effect severity, and OPAQ-SV physical function score. Compared to participants stable on therapy at entry, others had a higher risk, ranging from HR = 1.59 (95% CI: 1.36–1.85) for those new to therapy to HR = 2.00 (95% CI: 1.27–3.15) for those who recently augmented therapy at entry. Participants reporting moderate (HR = 1.31, 95% CI: 1.09–1.57) or severe (HR = 1.88, 95% CI: 1.49–2.39) side effects had a higher risk than those not reporting side effects. Participants reporting Osteoporosis Assessment Questionnaire-Short Version physical function scores in the lowest tertile had a higher risk (HR = 1.27, 95% CI: 1.07–1.52) than those reporting scores in the highest tertile.
Conclusion
Baseline osteoporosis medication transitions were common in the first year of POSSIBLE US™. Participants not on stable therapy at entry, or who reported severe side effects, or had poor physical health status were at higher risk for these transitions.


Similar content being viewed by others
References
Fletcher SW, Colditz GA (2002) Failure of estrogen plus progestin therapy for prevention. JAMA 288:366–368
Rossouw JE (2002) Effect of postmenopausal hormone therapy on cardiovascular risk. J Hypertens Suppl 20:S62–S65
Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ (2007) Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc 82:1493–1501
Cramer JA, Gold DT, Silverman SL, Lewiecki EM (2007) A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int 18:1023–1031
Downey TW, Foltz SH, Boccuzzi SJ, Omar MA, Kahler KH (2006) Adherence and persistence associated with the pharmacologic treatment of osteoporosis in a managed care setting. South Med J 99:570–575
Rossini M, Bianchi G, Di MO, Giannini S, Minisola S, Sinigaglia L, Adami S (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17:914–921
Kayser J, Ettinger B, Pressman A (2001) Postmenopausal hormonal support: discontinuation of raloxifene versus estrogen. Menopause 8:328–332
Barrett-Connor E, Ensrud K, Tosteson AN, Varon SF, Anthony M, Daizadeh N, Wade S (2009) Design of the POSSIBLE US™ Study: postmenopausal women's compliance and persistence with osteoporosis medications. Osteoporos Int 20:463–472
Atkinson MJ, Sinha A, Hass SL, Colman SS, Kumar RN, Brod M, Rowland CR (2004) Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes 2:12
Brooks R (1996) EuroQol: the current state of play. Health Policy 37:53–72
Randell AG, Bhalerao N, Nguyen TV, Sambrook PN, Eisman JA, Silverman SL (1998) Quality of life in osteoporosis: reliability, consistency, and validity of the Osteoporosis Assessment Questionnaire. J Rheumatol 25:1171–1179
Gallagher AM, Rietbrock S, Olson M, van Staa TP (2008) Fracture outcomes related to persistence and compliance with oral bisphosphonates. J Bone Miner Res 23:1569–1575
Cotte FE, Mercier F, De PG (2008) Relationship between compliance and persistence with osteoporosis medications and fracture risk in primary health care in France: a retrospective case-control analysis. Clin Ther 30:2410–2422
Siris ES, Selby PL, Saag KG, Borgstrom F, Herings RM, Silverman SL (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122:S3–S13
Burge R, wson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM, Pressman AR, Ettinger B (2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
McHorney CA, Schousboe JT, Cline RR, Weiss TW (2007) The impact of osteoporosis medication beliefs and side-effect experiences on non-adherence to oral bisphosphonates. Curr Med Res Opin 23:3137–3152
Ideguchi H, Ohno S, Takase K, Ueda A, Ishigatsubo Y (2008) Outcomes after switching from one bisphosphonate to another in 146 patients at a single university hospital. Osteoporos Int 19:1777–1783
Acknowledgments
The authors would like to acknowledge the other members of the POSSIBLE US™ Steering Committee: Elizabeth Barrett-Connor, Ted Ganiats, Marc Hochberg, Barbara Lukert, Robert Recker, Robert Rubin, and David Macarios. In addition, we are grateful for the methodologic and data analysis contributions of Mike Gao, Aalok Nadkar, Michael Damiata, and Richard Baumann. We would also like to acknowledge the REGISTRAT, Inc. staff that assisted with the implementation of this study and ongoing data collection as well as Michelle N Bradley of Amgen Inc. who provided editorial assistance. Funding for this study was provided by Amgen Inc., Thousand Oaks, CA USA.
Conflicts of interest
This study was funded by Amgen Inc., Thousand Oaks, CA, USA. Anna Tosteson provides consulting services to Amgen Inc. and Eli Lilly & Co. Thy P Do and Mary S Anthony are employees of Amgen Inc. Sally Wade provides consulting services to Amgen Inc. Robert W Downs receives research funding from and provides consulting services to Amgen Inc. The authors agree to allow the journal to review the primary data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tosteson, A.N.A., Do, T.P., Wade, S.W. et al. Persistence and switching patterns among women with varied osteoporosis medication histories: 12-month results from POSSIBLE US™. Osteoporos Int 21, 1769–1780 (2010). https://doi.org/10.1007/s00198-009-1133-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-1133-5