Abstract
Purpose
No systematic review has compared the clinical outcome of anterior stabilized ultra-congruent and standard cruciate-retaining inserts in fixed-bearing primary total knee arthroplasty. This study aimed to compare the outcomes and establish the superiority or equivalence of these inserts.
Methods
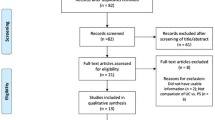
Pubmed, EMBASE, Medline, AMED, ERIC, and Proquest databases were searched electronically. PRISMA guidelines were followed in the conduct of the study. The clinical outcomes compared in the meta-analysis were overall knee score, WOMAC, score for knee function, score for knee pain, SF-12 PCS, knee flexion, manipulation under anaesthesia for postoperative knee stiffness, revision total knee arthroplasty or change of polyethylene insert for post-operative instability (relative risk [RR]) and survivorship. Study quality was evaluated using the Newcastle Ottawa Scale and the Modified Jadad scale.
Results
Fourteen studies comprising 9989 knees (three RCTs and 11 comparative case-cohort studies) were included for qualitative and quantitative analysis. The pooled analysis of the ultracongruent insert and the standard cruciate retaining insert was based on a cohort of 2860 and 7129 TKA, respectively. Knee pain was significantly better in patients that had standard inserts (p = 0.02; 95% CI − 1.06 to − 0.10), and the physical component of health-related quality of life was also significantly better in patients that had standard inserts (p = 0.02; 95% CI − 6.43 to − 0.64). There was a 72% lesser chance of revision TKA or change of insert for postoperative instability in knees that had been implanted with ultracongruent inserts (RR = 0.28; p = 0.0002; 95% CI 0.15–0.55). There was no difference in the otheroutcome measures. There was no significant difference between the two inserts, considering the minimal clinically important difference or absolute ratio.
Conclusion
Differences observed between the two types of inserts were not clinically significant. Therefore, based on current evidence, arthroplasty surgeons can use either of these inserts with cruciate-retaining knee prosthesis.
Level of evidence
Therapeutic study, Level II.







Similar content being viewed by others
References
Argenson JN, Boisgard S, Parratte S, Descamps S, Bercovy M, Bonnevialle P, Briard JL, Brilhault J, Chouteau J, Nizard R, Saragaglia D, Servien E, French Society of Orthopedic and Traumatologic Surgery (2013) Survival analysis of total knee arthroplasty at a minimum 10 years’ follow-up: a multicenter French nationwide study including 846 cases. Orthop Traumatol Surg Res 99(4):385–390
Bae JH, Yoon JR, Sung JH, Shin YS (2018) Posterior-stabilized inserts are preferable to cruciate-substituting ultracongruent inserts due to more favourable kinematics and stability. Knee Surg Sports Traumatol Arthrosc 26(11):3300–3310
Berend KR, Lombardi AV Jr, Adams JB (2013) Which total knee arthroplasty implant should I pick? Correcting the pathology: the role of knee bearing designs. Bone Joint J 95(11 Suppl A):129–132
Biyani R, Meneghini RM (2015) Component choices in primary knee arthroplasty. Semin Arthroplasty 26:202–205
Blevins JL, Chiu YF, Lyman S, Goodman SM, Mandl LA, Sculco PK, Figgie MP, McLawhorn AS (2019) Comparison of expectations and outcomes in rheumatoid arthritis versus osteoarthritis patients undergoing total knee arthroplasty. J Arthroplasty 34(9):1946–1952
Clement ND, Burnett R (2013) Patient satisfaction after total knee arthroplasty is affected by their general physical well-being. Knee Surg Sports Traumatol Arthrosc 21(11):2638–2646
Daniilidis K, Skwara A, Vieth V, Fuchs-Winkelmann S, Heindel W, Stückmann V, Tibesku CO (2012) Highly conforming polyethylene inlays reduce the in vivo variability of knee joint kinematics after total knee arthroplasty. Knee 19(4):260–265
Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS (2018) How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty 33(7S):71–75
Feyen H, Van Opstal N, Bellemans J (2013) Partial resection of the PCL insertion site during tibial preparation in cruciate-retaining TKA. Knee Surg Sports Traumatol Arthrosc 21(12):2674–2679
Fritzsche H, Beyer F, Postler A, Lützner J (2018) Different intraoperative kinematics, stability, and range of motion between cruciate-substituting ultracongruent and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26(5):1465–1470
Hafkamp FJ, Gosens T, de Vries J, den Oudsten BL (2020) Do dissatisfied patients have unrealistic expectations? A systematic review and best-evidence synthesis in knee and hip arthroplasty patients. EFORT Open Rev 5(4):226–240
Han HS, Kang SB (2020) Anterior-stabilized TKA is inferior to posterior-stabilized TKA in terms of postoperative posterior stability and knee flexion in osteoarthritic knees: a prospective randomized controlled trial with bilateral TKA. Knee Surg Sports Traumatol Arthrosc 28(10):3217–3225
Hofmann AA, Tkach TK, Evanich CJ, Camargo MP (2000) Posterior stabilization in total knee arthroplasty with use of an ultracongruent polyethylene insert. J Arthroplasty 15(5):576–583
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jones DP, Locke C, Pennington J, Theis JC (2006) The effect of sagittal laxity on function after posterior cruciate-retaining total knee arthroplasty. J Arthroplasty 21(5):719–723
Jones IA, Togashi R, Heckmann N, Vangsness CT Jr (2020) Minimal clinically important difference (MCID) for patient-reported shoulder outcomes. J Shoulder Elbow Surg 29(7):1484–1492
Kuo AC, Giori NJ, Bowe TR, Manfredi L, Lalani NF, Nordin DA, Harris AHS (2020) Comparing methods to determine the minimal clinically important differences in patient-reported outcome measures for veterans undergoing elective total hip or knee arthroplasty in Veterans Health Administration hospitals. JAMA Surg 155(5):404–411
Laigaard J, Pedersen C, Rønsbo TN, Mathiesen O, Karlsen APH (2021) Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: a systematic review. Br J Anaesth 126(5):1029–1037
Law JI, Hurst JM, Morris MJ, Berend KR, Lombardi AV Jr, Crawford DA (2021) Midterm outcomes and survivorship of anterior stabilized versus cruciate retaining bearing in primary total knee arthroplasty. J Arthroplasty 36(3):998–1002
Lee SS, Kim JH, Heo JW, Moon YW (2019) Gradual change in knee extension following total knee arthroplasty using ultracongruent inserts. Knee 26(4):905–913
Lizaur-Utrilla A, Gonzalez-Parreño S, Martinez-Mendez D, Miralles-Muñoz FA, Lopez-Prats FA (2020) Minimal clinically important differences and substantial clinical benefits for Knee Society Scores. Knee Surg Sports Traumatol Arthrosc 28(5):1473–1478
Lützner J, Firmbach FP, Lützner C, Dexel J, Kirschner S (2015) Similar stability and range of motion between cruciate-retaining and cruciate-substituting ultracongruent insert total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6):1638–1643
Maredupaka S, Meshram P, Chatte M, Kim WH, Kim TK (2020) Minimal clinically important difference of commonly used patient-reported outcome measures in total knee arthroplasty: review of terminologies, methods and proposed values. Knee Surg Relat Res 32(1):19
Mazzucchelli L, Deledda D, Rosso F, Ratto N, Bruzzone M, Bonasia DE, Rossi R (2016) Cruciate retaining and cruciate substituting ultra-congruent insert. Ann Transl Med 4(1):2
Meding JB, Meding LK, Meneghini RM, Malinzak RA (2021) Progressive tibial bearing sagittal plane conformity in cruciate-retaining total knee arthroplasty. J Arthroplasty 36(2):520–525
Mont MA, Costa CR, Naiziri Q, Johnson AJ (2013) Comparison of 2polyethlene inserts for a new cruciate-retaining total knee arthroplasty prosthesis. Orthopedics 36(1):33–35
Ng JWG, Bloch BV, James PJ (2019) Sagittal radius of curvature, trochlea design and ultracongruent insert in total knee arthroplasty. EFORT Open Rev 4(8):519–524
O’Donnell R, Brown K, Krueger V, Glasser J, Antoci V (2021) Comparing patient reported outcomes in depuy sigma curved versus curved plus polyethylene inserts in cruciate retaining total knee arthroplasty. J Orthop 24:54–57
Peters CL, Mulkey P, Erickson J, Anderson MB, Pelt CE (2014) Comparison of total knee arthroplasty with highly congruent anterior-stabilized bearings versus a cruciate-retaining design. Clin Orthop Relat Res 472(1):175–180
Rajgopal A, Aggarwal K, Khurana A, Rao A, Vasdev A, Pandit H (2017) Gait parameters and functional outcomes after total knee arthroplasty using Persona Knee System with cruciate retaining and Ultracongruent knee inserts. J Arthroplasty 32(1):87–91
Schwarzkopf R, Scott RD, Carlson EM, Currier JH (2015) Does increased topside conformity in modular total knee arthroplasty lead to increased backside wear? Clin Orthop Relat Res 473(1):220–225
Scott RD, Thornhill TS (1994) Posterior cruciate supplementing total knee arthroplasty using conforming inserts and cruciate recession. Effect on range of motion and radiolucent lines. Clin Orthop Relat Res 309:146–149
Song EK, Lim HA, Joo SD, Kim SK, Lee KB, Seon JK (2017) Total knee arthroplasty using ultracongruent inserts can provide similar stability and function compared with cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(11):3530–3535
Stirling P, Clement ND, MacDonald D, Patton JT, Burnett R, Macpherson GJ (2019) Early functional outcomes after condylar-stabilizing (deep-dish) versus standard bearing surface for cruciate-retaining total knee arthroplasty. Knee Surg Relat Res 31(1):3
Stronach BM, Adams JC, Jones LC, Farrell SM, Hydrick JM (2019) The effect of sacrificing the posterior cruciate ligament in total knee arthroplasties that use a highly congruent polyethylene component. J Arthroplasty 34(2):286–289
Totlis T, Iosifidis M, Melas I, Apostolidis K, Agapidis A, Eftychiakos N, Alvanos D, Kyriakidis A (2017) Cruciate-retaining total knee arthroplasty: How much of the PCL is really retained? Knee Surg Sports Traumatol Arthrosc 25(11):3556–3560
Uvehammer J, Regnér L, Kärrholm J (2001) Flat vs. concave tibial joint surface in total knee arthroplasty: randomized evaluation of 39 cases using radiostereometry. Acta Orthop Scand 72(3):257–265
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Wan HY, Li SY, Ji W, Yu B, Jiang N (2020) Fascia Iliaca compartment block for perioperative pain management of geriatric patients with hip fractures: a systematic review of randomized controlled trials. Pain Res Manag 2020:8503963
Yacovelli S, Grau LC, Hozack WJ, Courtney PM (2021) Functional outcomes are comparable between posterior stabilized and cruciate-substituting total knee arthroplasty designs at short-term follow-up. J Arthroplasty 36(3):986–990
Acknowledgements
The authors would like to thank Mr Ian Braithwaite (Consultant Spine Surgeon, Chester, United Kingdom) for the help in revising the manuscript.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors [KV, SK and RV] contributed to the study conception and design. Material preparation, data collection and analysis were performed by KV and SK. The first draft of the manuscript was written by KV and all authors commented on previous versions of the manuscript. All authors [KV, SK and RV] read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article
Ethics approval
The study protocol was reviewed by the Institutional Ethics Committee of Parul University, Vadodara (PUIECHR / PIMSR/ 00/ 081734/ 3913). It was granted exempt review since the study involved pooling and analysis of data that already exists in the public domain. There is no patient identifying information in the present manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vishwanathan, K., Kambhampati, S.B.S. & Vaishya, R. Equivalent outcomes of ultra-congruent and standard cruciate-retaining inserts in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30, 3076–3091 (2022). https://doi.org/10.1007/s00167-021-06833-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06833-z