Abstract
Purpose
To assess preferences among individuals aged ≥80 years for a future hypothetical critical illness requiring life-sustaining treatments.
Methods
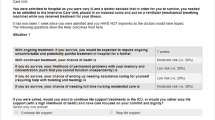
Observational cohort study of consecutive community-dwelling elderly individuals previously hospitalised in medical or surgical wards and of volunteers residing in nursing homes or assisted-living facilities. The participants were interviewed at their place of residence after viewing films of scenarios involving the use of non-invasive mechanical ventilation (NIV), invasive mechanical ventilation (IMV), and renal replacement therapy after a period of invasive mechanical ventilation (RRT after IMV). Demographic, clinical, and quality-of-life data were collected. Participants chose among four responses regarding life-sustaining treatments: consent, refusal, no opinion, and letting the physicians decide.
Results
The sample size was 115 and the response rate 87 %. Mean participant age was 84.8 ± 3.5 years, 68 % were female, and 81 % and 71 % were independent for instrumental activities and activities of daily living, respectively. Refusal rates among the elderly were 27 % for NIV, 43 % for IMV, and 63 % for RRT (after IMV). Demographic characteristics associated with refusal were married status for NIV [relative risk (RR), 2.9; 95 % confidence interval (95 %CI), 1.5–5.8; p = 0.002] and female gender for IMV (RR, 2.4; 95 %CI, 1.2–4.5; p = 0.01) and RRT (after IMV) (RR, 2.7; 95 %CI, 1.4–5.2; p = 0.004). Quality of life was associated with choices regarding all three life-sustaining treatments.
Conclusions
Independent elderly individuals were rather reluctant to accept life-sustaining treatments, especially IMV and RRT (after IMV). Their quality of life was among the determinants of their choices.

Similar content being viewed by others
References
Nguyen YL, Angus DC, Boumendil A, Guidet B (2011) The challenge of admitting the very elderly to intensive care. Ann Intensive Care 1:29
Boumendil A, Somme D, Garrouste-Orgeas M, Guidet B (2007) Should elderly patients be admitted to the intensive care unit? Intensive Care Med 33:1252–1262
Covinsky KE, Wu AW, Landefeld CS, Connors AF Jr, Phillips RS, Tsevat J, Dawson NV, Lynn J, Fortinsky RH (1999) Health status versus quality of life in older patients: does the distinction matter? Am J Med 106:435–440
Tabah A, Philippart F, Timsit JF, Willems V, Francais A, Leplege A, Carlet J, Bruel C, Misset B, Garrouste-Orgeas M (2010) Quality of life in patients aged 80 or over after ICU discharge. Crit Care 14:R2
Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, Papazian L (2011) Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care 15:R36
De Rooij SE, Govers AC, Korevaar JC, Giesbers AW, Levi M, De Jonge E (2008) Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Geriatr Soc 56:816–822
Ehlenbach WJ, Hough CL, Crane PK, Haneuse SJ, Carson SS, Curtis JR, Larson EB (2010) Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA 303:763–770
Boumendil A, Aergerter P, Garrouste-Orgeas M, Guitonneau AL, Menn AM, Ginsburg C, Davido A, Pateron D, Somme D, Simon D, Guidet B (2010) Tri des patients pour l’admission en réanimation à partir des urgences: que déclarent les médecins et que font-ils en pratique? Réanimation 19:SO52
Sprung CL, Carmel S, Sjokvist P, Baras M, Cohen SL, Maia P, Beishuizen A, Nalos D, Novak I, Svantesson M, Benbenishty J, Henderson B (2007) Attitudes of European physicians, nurses, patients, and families regarding end-of-life decisions: the ETHICATT study. Intensive Care Med 33:104–110
Coulter A (2007) Time for a change Health Expect 10:209–210
Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, Ferrier K, Payne S (2001) Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ 323:908–911
Roter D (1989) Which facets of communication have strong effects on outcome? A meta-analysis. In: Steward M (ed) Communicating with medical patients. Sage Publications, Newbury Park
Say R, Murtagh M, Thomson R (2006) Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns 60:102–114
Garrouste-Orgeas M, Montuclard L, Timsit JF, Misset B, Christias M, Carlet J (2003) Triaging patients to the ICU: a pilot study of factors influencing admission decisions and patient outcomes. Intensive Care Med 29:774–781
Philippart F, Timsit JF, Tabah A, Vesin A, Kpodji A, Durand-Gassellin B, Bruel C, Max A, Lau N, Misset B (2012) Avis des octogénaires pour une admission en réanimation: Etude ETHICA. Réanimation 21:S38–S39
David M, Starzec C (1996) Aisance à 60 ans, dépendance et isolement à 80 ans INSEE Première 447. http://www.insee.fr/fr/ffc/docs_ffc/ip447.pdf
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 31:721–727
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Power M, Quinn K, Schmidt S (2005) Development of the WHOQOL-old module. Qual Life Res 14:2197–2214
Skevington SM, Lotfy M, O’Connell KA (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 13:299–310
Lee J (1994) Odds ratio or relative risk for cross-sectional data? Int J Epidemiol 23:201–203
Garrouste-Orgeas M, Boumendil A, Pateron D, Aergerter P, Somme D, Simon T, Guidet B (2009) Selection of intensive care unit admission criteria for patients aged 80 years and over and compliance of emergency and intensive care unit physicians with the selected criteria: an observational, multicenter, prospective study. Crit Care Med 37:2919–2928
Garrouste-Orgeas M, Timsit JF, Montuclard L, Colvez A, Gattolliat O, Philippart F, Rigal G, Misset B, Carlet J (2006) Decision-making process, outcome, and 1-year quality of life of octogenarians referred for intensive care unit admission. Intensive Care Med 32:1045–1051
Van Mil AH, Van Klink RC, Huntjens C, Westendorp RG, Stiggelbout AM, Meinders AE, Lagaay AM (2000) Cardiopulmonary resuscitation preferences in Dutch community-dwelling and hospitalized elderly people: an interaction between gender and quality of life. Med Decis Making 20:423–429
Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG (2003) Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med 31:1901–1907
Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G (2012) Patient preferences for shared decisions: a systematic review. Patient Educ Couns 86:9–18
Formiga F, Chivite D, Ortega C, Casas S, Ramon JM, Pujol R (2004) End-of-life preferences in elderly patients admitted for heart failure. QJM 97:803–808
Fried TR, Bradley EH, Towle VR (2002) Assessment of patient preferences: integrating treatments and outcomes. J Gerontol B Psychol Sci Soc Sci 57:S348–S354
Fried TR, Bradley EH, Towle VR, Allore H (2002) Understanding the treatment preferences of seriously ill patients. N Engl J Med 346:1061–1066
Hansdottir H, Gruman C, Curry L, Judge JO (2000) Preferences for CPR among the elderly: the influence of attitudes and values. Conn Med 64:625–630
Hare J, Pratt C, Nelson C (1992) Agreement between patients and their self-selected surrogates on difficult medical decisions. Arch Intern Med 152:1049–1054
Kiphuth IC, Kohrmann M, Kuramatsu JB, Mauer C, Breuer L, Schellinger PD, Schwab S, Huttner HB (2010) Retrospective agreement and consent to neurocritical care is influenced by functional outcome. Crit Care 14:R144
Marco CA, Schears RM (2002) Societal opinions regarding CPR. Am J Emerg Med 20:207–211
Phillips RS, Wenger NS, Teno J, Oye RK, Youngner S, Califf R, Layde P, Desbiens N, Connors AF Jr, Lynn J (1996) Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Am J Med 100:128–137
Goodman MD, Tarnoff M, Slotman GJ (1998) Effect of advance directives on the management of elderly critically ill patients. Crit Care Med 26:701–704
Johnson RF Jr, Baranowski-Birkmeier T, O’Donnell JB (1995) Advance directives in the medical intensive care unit of a community teaching hospital. Chest 107:752–756
Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T (2007) Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc 55:189–194
Silveira MJ, Kim SY, Langa KM (2010) Advance directives and outcomes of surrogate decision making before death. N Engl J Med 362:1211–1218
Kish Wallace S, Martin CG, Shaw AD, Price KJ (2001) Influence of an advance directive on the initiation of life support technology in critically ill cancer patients. Crit Care Med 29:2294–2298
Smith SK, Dixon A, Trevena L, Nutbeam D, McCaffery KJ (2009) Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc Sci Med 69:1805–1812
Acknowledgments
We thank A. Wolfe, MD, for her assistance in preparing the manuscript. We are grateful to The French Society of Critical Care (SRLF) and Fondation de France for supporting this study. We thank Joelle Hedaya, Michel d’Urso, MD, Hélène Robbiani, MD, and Christine Richet for welcoming us in their nursing facilities to interview elderly individuals. This study was supported by the French Society for Critical Care (SRLF) and the Fondation de France. These organisations had no role in the design or conduct of the study; in data collection, management, or interpretation; or in the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Part II of the ETHICA Study can be found at: doi:10.1007/s00134-013-2977-x; an editorial discussing both parts of the ETHICA Study can be found at: doi:10.1007/s00134-013-2968-y.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Philippart, F., Vesin, A., Bruel, C. et al. The ETHICA study (part I): elderly’s thoughts about intensive care unit admission for life-sustaining treatments. Intensive Care Med 39, 1565–1573 (2013). https://doi.org/10.1007/s00134-013-2976-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2976-y