Abstract
Aims/hypothesis
The safety of metformin in heart failure has been questioned because of a perceived risk of life-threatening lactic acidosis, though recent studies have not supported this concern. We investigated the risk of all-cause mortality associated with individual glucose-lowering treatment regimens used in current clinical practice in Denmark.
Methods
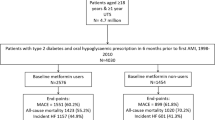
All patients aged ≥30 years hospitalised for the first time for heart failure in 1997–2006 were identified and followed until the end of 2006. Patients who received treatment with metformin, a sulfonylurea and/or insulin were included and assigned to mono-, bi- or triple therapy groups. Multivariable Cox proportional hazard regression models were used to assess the risk of all-cause mortality.
Results
A total of 10,920 patients were included. The median observational time was 844 days (interquartile range 365–1,395 days). In total, 6,187 (57%) patients died. With sulfonylurea monotherapy used as the reference, adjusted hazard ratios for all-cause mortality associated with the different treatment groups were as follows: metformin 0.85 (95% CI 0.75–0.98, p = 0.02), metformin + sulfonylurea 0.89 (95% CI 0.82–0.96, p = 0.003), metformin + insulin 0.96 (95% CI 0.82–1.13, p = 0.6), metformin + insulin + sulfonylurea 0.94 (95% CI 0.77–1.15, p = 0.5), sulfonylurea + insulin 0.97 (95% CI 0.86–1.08, p = 0.5) and insulin 1.14 (95% CI 1.06–1.20, p = 0.0001).
Conclusions/interpretation
Treatment with metformin is associated with a low risk of mortality in diabetic patients with heart failure compared with treatment with a sulfonylurea or insulin.
Similar content being viewed by others
Introduction
Heart failure (HF) patients comprise a particular group of diabetic patients in whom the optimal pharmacological glucose-lowering treatment regimen remains insecure. In particular, the safety of metformin administration has been questioned because of a perceived risk of life-threatening lactic acidosis. At the same time, however, metformin has been hypothesised to improve outcomes, for example by reducing insulin resistance, which has shown to be an independent and important key factor for HF development and deterioration [1, 2]. Mechanistically, insulin resistance is associated with a disproportionately increased cardiac fatty acid metabolism relative to glucose consumption and, while these abnormalities may not compromise basal cardiomyocyte energy supply, they may be inadequate to meet energy requirements when additional cardiac stressors such as pressure/volume overload and tachycardia are present [3, 4]. Inappropriate upregulation of compensatory mechanisms, for example activation of the renin–angiotensin–aldosterone system and vasopressin release, may then worsen HF [3].
From an epidemiological view, the presence of diabetes in HF populations increases the risk of death by 30–50% [5–7]. Thus, increased knowledge about the outcomes associated with different glucose-lowering agents in this particular high-risk group is important. The aim of the present study was therefore to specifically address the outcomes associated with the most commonly used glucose-lowering agents in Denmark, namely metformin, sulfonylureas and/or insulin in an unselected nationwide cohort of HF patients.
Methods
Data acquisition
Because of the unique and permanent civil registration numbers held by all Danish citizens and a government-financed healthcare system, Denmark has several unique and complete nationwide healthcare registers. The present study was based on individual-level linkage of data from three of these registers. The Danish National Patient Register included data on all hospitalisations since 1978. Available variables included time of admission and discharge, and primary and secondary hospitalisation-discharge diagnoses. All diagnoses were coded according to the International Classification of Diseases (the 8th revision [ICD-8] between 1978 and 1993, and the 10th revision [ICD-10; www.who.int/classifications/icd/en/] from 1994). The diagnosis of HF has a specificity of 99% in the register, a sensitivity of 29% and a positive predictive value of 81% [8]. The Danish Register of Medicinal Product Statistics held information on all dispensed prescriptions from Danish pharmacies since 1995. The data available included dispensing date, strength and quantity dispensed. All drugs were registered according to the Anatomical Therapeutic Chemical (ATC) classification system. The register has been shown to be complete and accurate [9]. The National Causes of Death Register held information on dates of occurrence and primary and contributing causes of death.
Population
All patients aged ≥30 years and hospitalised for HF (ICD-10 codes I50, I42, J81.9 and I11.0) in the period between 1997 and 2006 were identified. To create a population with homogeneous HF history, patients with previous hospitalisations for HF during the period from 1978 until 1996 (diagnosis codes [ICD-10] I50, I42, J81, I11.0 and [ICD-8] 425, 4270, 4271) were excluded from the study. Those who were alive 30 days after discharge and were receiving treatment with metformin (ATC code A10BA02), sulfonylureas (ATC code A10BB) and/or insulin (ATC code A10A) formed the present study population. A further requirement was prior use of any of these agents within 90 days preceding HF hospitalisation, ensuring that all patients suffered from diabetes prior to HF hospitalisation. Patients with concomitant use of alpha-glucosides (ATC code A10BF) or thiazolidinediones (ATC code A10BG) were not included, primarily because only a small number of patients were using these agents. Baseline treatment groups were defined by the respective glucose-lowering agents used at day 30 after discharge.
Study start and endpoints
The observational starting time point was defined as 30 days after discharge. This time point was chosen because of concerns about significant changes in medical therapy during hospitalisation, and previous work has demonstrated that in patients hospitalised for HF treatment is initiated in proximity to discharge [10].
The primary study endpoint was all-cause mortality. The population was followed until the end of 2006, giving a maximal follow-up time of 10 years. Due to the prevailing concerns regarding risk of lactic acidosis by metformin, hospitalisation or death due to lactic acidosis were also studied (ICD-10 codes E872A, E872B and E872D). In addition, the proportion of patients dying from cancer (ICD-10 codes C00–C97), diabetes-related conditions (ICD-10 codes E10–E14) and cardiovascular causes (ICD-10 codes I00–I99) were specified.
Identification of pharmacotherapy and concomitant diseases
By determining the amount of dispensed tablets, their strengths and the dispensing-time interval for up to seven consecutively claimed prescriptions, an individually adjusted coverage of drug treatment was calculated for metformin and sulfonylureas. This method has been described in detail previously by Gislason et al. and Fosbol et al. [11, 12] Loop diuretic dosages used at study baseline were calculated by the same method and individual loop diuretic dosages were used as a proxy for the severity of HF, as reported previously by Gislason et al. (dosages grouped in: <40 mg/day; 40−<80 mg/day; 80−<160 mg/day; and ≥160 mg/day) [10]. Supporting the use of such proxy measures, previous work by Eshaghian et al. has demonstrated that loop diuretic dosages correlate with the risk of mortality, peak oxygen uptake and New York Heart Association functional class, but not with creatinine clearance, in patients with HF [13]. Patients were classified as insulin users from the date of the first claimed prescription of insulin until the end of the study, as patients initiated on insulin usually need lifelong treatment.
Concomitant medical therapy was defined by claimed prescriptions during the period of 90 days prior to hospitalisation until 30 days after discharge using the following agents (ATC codes): beta-blockers (C07), lipid-lowering drugs (C10A), angiotensin-converting-enzyme inhibitors and angiotensin-2-receptor blockers (C09), thiazides (C03A), spironolactone (C03D), calcium channel blockers (C08), digoxin (C01AA05), vitamin K antagonists (B01AA0), aspirin (B01AC06) and clopidogrel (B01AC04), as used previously by Gislason et al. [10].
Comorbidity was defined by primary or secondary hospitalisation diagnoses up to 1 year prior to HF hospitalisation. A modified version of the Charlson index for ICD-10 (exclusion of the diabetes and HF diagnoses) was used [14].
Statistics
Continuous variables were compared with the t test and discrete variables were compared with the χ 2 test. The Cochran–Armitage trend test was used to test the trends in treatment over calendar time. Median observational time was calculated based on patients who did not die during the study period. Cox proportional hazard models were used for analyses of mortality rates with sulfonylurea monotherapy used as reference. All analyses investigating the risk of all-cause mortality were adjusted for calendar year of index hospitalisation, age, sex, Charlson index, diabetic complications, concomitant cardiovascular pharmacotherapy and dosage of loop diuretics. The main analysis was carried out according to baseline treatment groups, but to ensure that the initial findings were not significantly influenced by changes in treatment over time, an additional time-dependent Cox analysis was performed. Use of glucose-lowering agents was continuously updated and patients were allowed to change treatment group over time (or to be classified as out of treatment). Because of possible fluctuations in medical therapy immediately prior to death, we used a time-lagged approach of 90 days [15].
As patients using and not using insulin may not be completely comparable, we performed stratified subgroup analyses according to insulin treatment to ensure the robustness of our findings. Further, because clinicians might be less likely to prescribe metformin than other glucose-lowering agents for patients with more severe diabetes and HF, we also performed survival analyses on 1:1 propensity score-matched subpopulations comprising patients using: (1) metformin or sulfonylurea as monotherapy; (2) metformin + sulfonylurea or sulfonylurea as monotherapy; and (3) metformin + insulin or insulin as monotherapy at baseline. The propensity for metformin treatment at baseline was acquired by multivariable logistic regression analysis conditional on baseline characteristics. The models had good discriminatory power, with c-statistics ranging from 0.71 to 0.79. Patients receiving metformin were then matched with controls by the propensity score using the Greedy matching macro (Mayo Clinic College of Medicine; http://mayoresearch.mayo.edu/biostat/upload/gmatch.sas, last accessed 1 April 2009).
All analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC, USA).
Ethics
The study was approved by the Danish Data Protection Agency (No. 2007-41-1667). In Denmark, register-based studies in which individuals cannot be identified do not require ethical approval.
Results
Population
Among the total of 10,920 patients with a first diagnosis of HF and concomitant diabetes included in the present study, 2,952 (27%) were treated with metformin at baseline (Table 1). Patients using metformin were younger than patients not using metformin, mean age 70 (SD 10) years and 73 (SD 11) years, respectively (p < 0.0001). Compared with patients not using metformin, metformin users had a lower prevalence of renal diseases (2% vs 6%, p < 0.0001) and were more likely to be male (58% vs 55%, p = 0.008). The proportions of patients having diabetes for more than 2 years were comparable among metformin monotherapy and sulfonylurea monotherapy groups (60% vs 57%, p = 0.14). The prevalence of ischaemic heart disease and a history of acute myocardial infarction did not differ among those using metformin vs those not using metformin (30% vs 32%, p = 0.3, and 15% vs 17%, p = 0.2, respectively). The patterns of use of metformin and insulin increased over the study period, whereas the use of sulfonylureas decreased (p for trends <0.0001).
All-cause mortality
The median observational time was 844 days (interquartile range [IQR] 365–1,395 days) and a total number of 6,187 (57%) patients died. Table 2 presents the crude numbers of deaths and death rates for each of the studied groups. The adjusted hazard ratios for all-cause mortality associated with the different treatment modalities are presented in Fig. 1. Compared with sulfonylureas as monotherapy, metformin as monotherapy and metformin in combination with sulfonylureas were associated with an improved outcome (hazard ratios for death compared with sulfonylurea monotherapy were 0.85 [95% CI 0.75–0.98, p = 0.02] for metformin monotherapy and 0.89 [0.82–0.96, p = 0.003] for metformin + sulfonylurea). The effect of metformin was similar in women and men (p for interaction = 0.8), did not differ according to year of hospitalisation (p for interaction between calendar year and metformin = 0.8), was not found to be dependent on age (p for interaction between age and metformin = 0.3) and was not dependent on concomitant use of insulin or sulfonylureas (p for interactions = 0.8 and 0.1).
Sensitivity analyses
Separate analyses of patients using and not using insulin found similar results to those of the main analysis. In patients not using insulin, metformin monotherapy was associated with an HR of 0.89 (0.78–1.02) and the use of sulfonylurea + metformin 0.90 (0.83–0.98), compared with the use of sulfonylureas as monotherapy. Correspondingly, use of metformin + insulin was associated with an HR of 0.96 (0.79–1.15), use of metformin + sulfonylurea + insulin 0.96 (0.77–1.19) and use of insulin monotherapy 1.17 (1.04–1.30), compared with use of sulfonylurea + insulin.
The time-dependent Cox analysis found similar results as the main analysis and are presented in Fig. 2.
The propensity score-matched subgroup analyses included 1,274, 2,926 and 930 patients in metformin monotherapy or sulfonylurea monotherapy groups (Fig. 3a); metformin + sulfonylurea or sulfonylurea monotherapy groups (Fig. 3b); and metformin + insulin or insulin monotherapy groups (Fig. 3c). There were no differences between cases and controls in any baseline characteristic (p for differences between groups >0.05 for all variables, see Electronic supplementary material [ESM]). The median observational times were 748 (IQR 347–1,302), 1,092 (507–1,847), and 601 (260–1,246) days for the respective subgroup analyses. As illustrated, users of metformin were found to have a lower mortality than controls in all three analyses.
Kaplan–Meier mortality curves for subgroups of patients treated with (a) metformin monotherapy (black line) vs sulfonylurea monotherapy (grey line); (b) metformin + sulfonylurea (black line) vs sulfonylurea monotherapy (grey line); and (c) metformin + insulin (black line) vs insulin monotherapy (grey line). All subgroups were matched on baseline characteristics. Logrank p < 0.05 for all three analyses
Specific causes of death
As shown in Table 2, approximately 55% of all deaths had a cardiovascular cause, 36% involved diabetes and 11% involved cancer. In total, 83% of all deaths involved any of these conditions. Compared with patients using sulfonylurea monotherapy, patients using metformin as monotherapy had a significantly lower risk of death from diabetes or cardiovascular causes while the risk was significantly higher in patients using insulin as monotherapy.
Lactic acidosis
No hospitalisations or deaths attributed to lactic acidosis were identified over the study period.
Discussion
The present study, comprising all Danish patients who were hospitalised with HF for the first time during 1997–2006 and treated with metformin, sulfonylureas and/or insulin, demonstrated that use of metformin was associated with a lower mortality compared with use of insulin or sulfonylureas. Although other studies have found similar results [16, 17], the present study, based on an unselected and nationwide population, contributes substantially to the evidence demonstrating that, in current practice, metformin is not associated with increased risk of death or lactic acidosis in patients with HF.
In patients without HF, current evidence points towards better clinical outcomes with metformin treatment compared with most of the sulfonylureas, and the recent clinical guidelines by the American Diabetes Association recommend that all patients with newly developed type 2 diabetes and a creatinine clearance >30 ml min−1 m−2 are initiated on metformin [18]. It seems appropriate to also apply these recommendations to patients with HF, as the major reason for questioning metformin safety in this particular group has been concerns regarding the risk of lactic acidosis. Notably, we found no hospitalisations or deaths attributable to lactic acidosis and our findings therefore support recent reviews that have concluded that concerns for lactic acidosis associated with metformin treatment may not be justified [19, 20]. It should, however, be noted that the sensitivity of the lactic acidosis diagnosis in our registers is unknown, but because the mortality for lactic acidosis is very high, it appears unlikely that lactic acidosis occurred frequently.
In our sensitivity analyses of matched populations, the use of metformin was associated with a reduced risk of all-cause mortality across all the studied groups and it is possible that metformin has a direct positive effect on HF progression and thereby survival. For example, metformin has been shown to delay the progression of ischaemic cardiomyopathy in mice after myocardial infarction [21] and to attenuate the progression of pace-induced HF in dogs [22]. Such a hypothesis has, however, never been challenged in a randomised clinical trial. In 2006, Eurich et al. initiated a pilot study to compare metformin with placebo in HF patients with diabetes [23]. Unfortunately, during a screening period of 6 months, these investigators found too few patients eligible for study inclusion, the main reason being that study candidates were already in treatment with metformin and they concluded that such a randomised clinical trial would be virtually impossible to conduct [23]. Data from the present study, including patients hospitalised in 1997–2006, showed a temporal increase in the use of metformin and a temporal decrease in the use of sulfonylureas. It therefore appears unlikely that future randomised clinical trials will be conducted to further delineate the outcomes with metformin in this patient group. Therefore, the present data and results of other related epidemiological studies, which have shown that metformin is not associated with an increased risk of death in heart failure patients [16, 17], probably represents the highest achievable level of evidence on this particular subject.
Strengths and limitations
The major strengths include the large and unselected cohort of HF patients as well as the long study period. The government-financed healthcare coverage of all inhabitants and partial reimbursement of drug expenses ensured the completeness of data registers. Moreover, selection bias in relation to age, participation in the labour market, social status etc. should be limited due to the universal healthcare access in Denmark. However, it should be noted that the sensitivity of the HF diagnosis in our registers is 29% and therefore the present analysis is based on only a subgroup of all HF patients in Denmark [8]. Furthermore, the positive predictive value of the heart failure diagnosis is 81% in our registers [8], which may be considered to be acceptable, although it cannot be excluded that the 19% who do not have heart failure may blur the picture.
Despite thorough adjustments for differences in comorbidity and concomitant pharmacotherapy, we acknowledge the possible effect of unmeasured confounders. In particular, data on body mass index, blood pressure, HbA1c levels, diabetes duration, smoking habits, lipid profiles, brain natriuretic peptide concentrations, creatinine clearance and echocardiography variables, such as left ventricular function, were lacking. Therefore, some degree of residual and hidden confounding by indication with those receiving metformin potentially being healthier than those not receiving metformin cannot be excluded. Finally, we were unable to discern between type 1 and type 2 diabetes, but this was probably of minor significance, as a recent large Danish study of consecutively admitted HF patients in 2001–2002 found that only 2% of patients with diabetes suffered from the type 1 form [24]. The proportion of patients with type 1 diabetes in the present study was therefore presumed to be small.
Conclusion and clinical implications
Treatment with metformin is associated with a low risk of mortality in diabetic patients with HF, as compared with treatment with sulfonylureas or insulin. Inclusion of metformin in glucose-lowering treatment regimens in HF patients may provide long-term benefits.
Abbreviations
- ATC:
-
Anatomical therapeutic chemical
- HF:
-
Heart failure
- ICD:
-
International classification of diseases
- IQR:
-
Interquartile range
References
Ingelsson E, Sundstrom J, Arnlov J, Zethelius B, Lind L (2005) Insulin resistance and risk of congestive heart failure. JAMA 294:334–341
Kalogeropoulos A, Georgiopoulou V, Harris TB et al (2009) Glycemic status and incident heart failure in elderly without history of diabetes mellitus: the health, aging, and body composition study. J Card Fail 15:593–599
Witteles RM, Fowler MB (2008) Insulin-resistant cardiomyopathy clinical evidence, mechanisms, and treatment options. J Am Coll Cardiol 51:93–102
Young ME, McNulty P, Taegtmeyer H (2002) Adaptation and maladaptation of the heart in diabetes: part II: potential mechanisms. Circulation 105:1861–1870
Domanski M, Krause-Steinrauf H, Deedwania P et al (2003) The effect of diabetes on outcomes of patients with advanced heart failure in the BEST trial. J Am Coll Cardiol 42:914–922
Gustafsson I, Brendorp B, Seibaek M et al (2004) Influence of diabetes and diabetes–gender interaction on the risk of death in patients hospitalized with congestive heart failure. J Am Coll Cardiol 43:771–777
Kannel WB, Hjortland M, Castelli WP (1974) Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol 34:29–34
Kumler T, Gislason GH, Kirk V et al (2008) Accuracy of a heart failure diagnosis in administrative registers. Eur J Heart Fail 10:658–660
Gaist D, Sorensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44:445–448
Gislason GH, Rasmussen JN, Abildstrom SZ et al (2007) Persistent use of evidence-based pharmacotherapy in heart failure is associated with improved outcomes. Circulation 116:737–744
Fosbol EL, Gislason GH, Jacobsen S et al (2009) Risk of myocardial infarction and death associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs) among healthy individuals: a nationwide cohort study. Clin Pharmacol Ther 85:190–197
Gislason GH, Rasmussen JN, Abildstrom SZ et al (2006) Long-term compliance with beta-blockers, angiotensin-converting enzyme inhibitors, and statins after acute myocardial infarction. Eur Heart J 27:1153–1158
Eshaghian S, Horwich TB, Fonarow GC (2006) Relation of loop diuretic dose to mortality in advanced heart failure. The Am J Cardiol 97:1759–1764
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Fisher LD, Lin DY (1999) Time-dependent covariates in the Cox proportional-hazards regression model. Annu Rev Public Health 20:145–157
Eurich DT, McAlister FA, Blackburn DF et al (2007) Benefits and harms of antidiabetic agents in patients with diabetes and heart failure: systematic review. BMJ 335:497
Masoudi FA, Inzucchi SE, Wang Y, Havranek EP, Foody JM, Krumholz HM (2005) Thiazolidinediones, metformin, and outcomes in older patients with diabetes and heart failure: an observational study. Circulation 111:583–590
Nathan DM, Buse JB, Davidson MB et al (2009) Medical management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 52:17–30
Khurana R, Malik IS (2010) Metformin: safety in cardiac patients. Heart 96:99–102
Tahrani AA, Varughese GI, Scarpello JH, Hanna FW (2007) Metformin, heart failure, and lactic acidosis: is metformin absolutely contraindicated? BMJ 335:508–512
Gundewar S, Calvert JW, Jha S et al (2009) Activation of AMP-activated protein kinase by metformin improves left ventricular function and survival in heart failure. Circ Res 104:403–411
Sasaki H, Asanuma H, Fujita M et al (2009) Metformin prevents progression of heart failure in dogs: role of AMP-activated protein kinase. Circulation 119:2568–2577
Eurich DT, Tsuyuki RT, Majumdar SR et al (2009) Metformin treatment in diabetes and heart failure: when academic equipoise meets clinical reality. Trials 10:12
Andersson C, Weeke P, Pecini R et al (2010) Long-term impact of diabetes in patients hospitalized with ischemic and non-ischemic heart failure. Scand Cardiovasc J 44:37–44
Acknowledgements
The study was supported by research grant from the Danish Agency for Science, Technology and Innovation (Grant no. 271-08-0944). The funding source had no influence on study design, data analysis, interpretation or writing of the manuscript.
Duality of interest
A. Vaag is employed by Steno Diabetes Center, which is owned by Novo Nordisk. Other authors report no duality of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 89 kb)
Rights and permissions
About this article
Cite this article
Andersson, C., Olesen, J.B., Hansen, P.R. et al. Metformin treatment is associated with a low risk of mortality in diabetic patients with heart failure: a retrospective nationwide cohort study. Diabetologia 53, 2546–2553 (2010). https://doi.org/10.1007/s00125-010-1906-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1906-6