Abstract
Background
Acute cholecystitis (AC), frequently responsible for presentation to the emergency department, requires expedient diagnosis and definitive treatment by a general surgeon. Ultrasonography, usually performed by radiology technicians and reported by radiologists, is the first-line imaging study for the assessment of AC. Targeted point-of-care ultrasound (POCUS), particularly in the hands of the treating surgeon, may represent an evolution in surgical decision-making and may expedite care, reducing morbidity and cost.
Methods
This consensus guideline was written under the auspices of the European Society of Trauma and Emergency Surgery (ESTES) by the POCUS working group. A systematic literature search identified relevant papers on the diagnosis and treatment of AC. Literature was critically-appraised according to the GRADE evidence-based guideline development method. Following a consensus conference at the European Congress of Trauma & Emergency Surgery (Valencia, Spain, May 2018), final recommendations were approved by the working group, using a modified e-Delphi process, and taking into account the level of evidence of the conclusion.
Recommendations
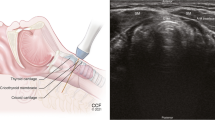
We strongly recommend the use of ultrasound as the first-line imaging investigation for the diagnosis of AC; specifically, we recommend that POCUS may be adopted as the primary imaging adjunct to surgeon-performed assessment of the patient with suspected AC. In line with the Tokyo guidelines, we strongly recommend Murphy’s sign, in conjunction with the presence of gallstones and/or wall thickening as diagnostic of AC in the correct clinical context. We conditionally recommend US as a preoperative predictor of difficulty of cholecystectomy. There is insufficient evidence to recommend contrast-enhanced ultrasound or Doppler ultrasonography in the diagnosis of AC. We conditionally recommend the use of ultrasound to guide percutaneous cholecystostomy placement by appropriately-trained practitioners.
Conclusions
Surgeons have recently embraced POCUS to expedite diagnosis of AC and provide rapid decision-making and early treatment, streamlining the patient pathway and thereby reducing costs and morbidity.



Similar content being viewed by others
Change history
08 November 2019
Unfortunately, the author Luca Ponchietti was omitted in the original publication. Please find the correct author list here.
References
Zacks S. A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol. 2002;97(2):334–40.
Keus F, de Jong J, Gooszen H, Laarhoven C. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Datab Syst Rev. 2004;2006:4.
Chau C, Tang C, Ha P, Kwok S, Yau K, Li M, et al. Laparoscopic cholecystectomy for acute cholecystitis: the evolving trend in an institution. Asian J Surg. 2006;29(3):120–4.
Malla B, Shrestha R. Laparoscopic cholecystectomy: complication and conversion rate. Kathmandu Univ Med J. 2012;8:4.
Sanjay P, Weerakoon R, Shaikh I, Bird T, Paily A, Yalamarthi S. A 5-year analysis of readmissions following elective laparoscopic cholecystectomy—cohort study. Int J Surg. 2011;9(1):52–4.
Lengyel B, Azagury D, Varban O, Panizales M, Steinberg J, Brooks D, et al. Laparoscopic cholecystectomy after a quarter century: why do we still convert? Surg Endosc. 2011;26(2):508–13.
Unawane A, Kamyab A, Patel M, Flynn J, Mittal V. Changing paradigms in minimally invasive surgery training. Am J Surg. 2013;205(3):284–8.
Gutt C, Encke J, Köninger J, Harnoss J, Weigand K, Kipfmüller K, et al. Acute cholecystitis. Ann Surg. 2013;258(3):385–93.
Rumack C. Diagnostic ultrasound. 5th ed. Amsterdam: Elsevier Science; 2018.
Hameed M, Sahu A, Ali H, Raje D, Sheth H. The diagnostic utility of ultrasound for acute cholecystitis. Clin Radiol. 2016;71:S27.
Adams J, Barton E. Emergency medicine: clinical essentials. Amsterdam: Elsevier Health Sciences; 2013.
Woo M, Taylor M, Loubani O, Bowra J, Atkinson P. My patient has got abdominal pain: identifying biliary problems. Ultrasound. 2014;22(4):223–8.
Pereira J, Afonso A, Constantino J, Matos A, Henriques C, Zago M, et al. Accuracy of ultrasound in the diagnosis of acute cholecystitis with coexistent acute pancreatitis. Eur J Trauma Emerg Surg. 2015;43(1):79–83.
Townsend C, Evers B, Mattox K, Beauchamp R. Sabiston textbook of surgery. Philadelphia: Elsevier; 2017.
Zieleskiewicz L, Muller L, Lakhal K, Meresse Z, Arbelot C, Bertrand P, et al. Point-of-care ultrasound in intensive care units: assessment of 1073 procedures in a multicentric, prospective, observational study. Intensive Care Med. 2015;41(9):1638–47.
Parks A, Atkinson P, Verheul G, LeBlanc-Duchin D. Can medical learners achieve point-of-care ultrasound competency using a high-fidelity ultrasound simulator?: a pilot study. Crit Ultrasound J. 2013;5(1):9.
Blanco P, Volpicelli G. Common pitfalls in point-of-care ultrasound: a practical guide for emergency and critical care physicians. Crit Ultrasound J. 2016;8:1.
Bhagra A, Tierney D, Sekiguchi H, Soni N. Point-of-Care ultrasonography for primary care physicians and general internists. Mayo Clin Proc. 2016;91(12):1811–27.
Moore C, Copel J. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–57.
Kotagal M, Quiroga E, Ruffatto B, Adedipe A, Backlund B, Nathan R, et al. Impact of point-of-care ultrasound training on surgical residents’ confidence. J Surg Educ. 2015;72(4):e82–7.
Mollenkopf M, Tait N. Is it time to include point-of-care ultrasound in general surgery training? A review to stimulate discussion. ANZ J Surg. 2013;83(12):908–11.
Yokoe M, Hata J, Takada T, Strasberg S, Asbun H, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepato-Biliary-Pancreat Sci. 2018;25(1):41–54.
Takada T, Strasberg S, Solomkin J, Pitt H, Gomi H, Yoshida M, et al. TG13: updated Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepato-Biliary-Pancreat Sci. 2013;20(1):1–7.
Hirota M, Takada T, Kawarada Y, Nimura Y, Miura F, Hirata K, et al. Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo guidelines. J Hepato-Biliary-Pancreat Surg. 2007;14(1):78–82.
Delphi Technique. https://methods.sagepub.com/Reference/encyc-of-research-design. 2018. Accessed 3 Jan 2018.
Gradepro [Internet]. Gradepro.org. 2018. https://gradepro.org/resources/. Accessed 21 Dec 2018.
Herring W. Learning radiology. 3rd ed. Philadelphia: Elsevier; 2015.
Kiewiet J, Leeuwenburgh M, Bipat S, Bossuyt P, Stoker J, Boermeester M. A systematic review and meta-analysis of diagnostic performance of imaging in acute cholecystitis. Radiology. 2012;264(3):708–20.
Blaivas M, Adhikari S. Diagnostic utility of cholescintigraphy in emergency department patients with suspected acute cholecystitis: comparison with bedside RUQ ultrasonography. J Emerg Med. 2007;33(1):47–52.
Kaoutzanis C, Davies E, Leichtle S, Welch K, Winter S, Lampman R, et al. Abdominal ultrasound versus hepato-imino diacetic acid scan in diagnosing acute cholecystitis—what is the real benefit? J Surg Res. 2018;188:44–52.
Klugsberger B, Haslinger-Eisterer B, Oppelt P, Shamiyeh A. Clinical value of sonography and CT-scan in the diagnosis of acute cho-lecystitis: a retrospective analysis. Ann Emerg Surg. 2017;2(4):1021.
O’Connor O, Maher M. Imaging of cholecystitis. Am J Roentgenol. 2011;196(4):W367–74.
Elsayes K, Oliveira E, Narra V, EL-Merhi F, Brown J. Magnetic resonance imaging of the gallbladder: spectrum of abnormalities. Acta Radiol. 2007;48(5):476–82.
Ansaloni L, Pisano M, Coccolini F, Peitzmann A, Fingerhut A, Catena F, et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg. 2016;11:1.
Warttig S, Ward S, Rogers G. Diagnosis and management of gallstone disease: summary of NICE guidance. BMJ. 2014;349(13):g6241.
Lammert F, et al. EASL clinical practice guidelines on the prevention diagnosis and treatment of gallstones. J Hepatol. 2016;65(1):146–81.
Yokoe M, Takada T, Hwang T, Endo I, Akazawa K, Miura F, et al. Descriptive review of acute cholecystitis: Japan-Taiwan collaborative epidemiological study. J Hepato-Biliary-Pancreat Sci. 2017;24(6):319–28.
Cetinkunar S, Erdem H, Aktimur R, Soker G, Bozkurt H, Reyhan E, et al. Evaluation of power Doppler sonography in acute cholecystitis to predict intraoperative findings: prospective clinical study. Turkish J Trauma Emerg Surg. 2014;2014:51–6.
Soyer P, Brouland J, Boudiaf M, Kardache M, Pelage J, Panis Y, et al. Color velocity imaging and power Doppler sonography of the gallbladder wall: a new look at sonographic diagnosis of acute cholecystitis. Am J Roentgenol. 1998;171(1):183–8.
Paulson E, Kliewer M, Hertzberg B, Paine S, Carroll B. Diagnosis of acute cholecystitis with color Doppler sonography: significance of arterial flow in thickened gallbladder wall. Am J Roentgenol. 1994;162(5):1105–8.
Uggowitzer M, Kugler C, Schramayer G, Kammerhuber F, Gröll R, Hausegger K, et al. Sonography of acute cholecystitis: comparison of color and power Doppler sonography in detecting a hypervascularized gallbladder wall. Am J Roentgenol. 1997;168(3):707–12.
Tessler F, Tublin M. Blood flow in healthy gallbladder walls on color and power Doppler sonography: effect of wall thickness and gallbladder volume. Am J Roentgenol. 1999;173(5):1247–9.
Adamietz B, Wenkel E, Uder M, Meyer T, Schneider I, Dimmler A, et al. Contrast enhanced sonography of the gallbladder: a tool in the diagnosis of cholecystitis? Eur J Radiol. 2007;61(2):262–6.
Ripollés T, Martínez-Pérez M, Martin G, Vizuete J, Martínez-García R, Diez J, et al. Usefulness of contrast-enhanced US in the diagnosis of acute gangrenous cholecystitis: a comparative study with surgical and pathological findings. Eur J Radiol. 2016;85(1):31–8.
Sagrini E, Pecorelli A, Pettinari I, Cucchetti A, Stefanini F, Bolondi L, et al. Contrast-enhanced ultrasonography to diagnose complicated acute cholecystitis. Intern Emerg Med. 2015;11(1):19–30.
Kawai R, Hata J, Manabe N, Imamura H, Iida A, Nakatou R, et al. Contrast-enhanced ultrasonography with Sonazoid for diagnosis of gangrenous cholecystitis. J Med Ultrason. 2015;43(2):193–9.
Martínez A, Bona X, Velasco M, Martín J. Diagnostic accuracy of ultrasound in acute cholecystitis. Gastroint Radiol. 1986;11(1):334–8.
Ralls P, Colletti P, Lapin S, Chandrasoma P, Boswell W, Ngo C, et al. Real-time sonography in suspected acute cholecystitis. Prospective evaluation of primary and secondary signs. Radiology. 1985;155(3):767–71.
Bree R. Further observations on the usefulness of the sonographic Murphy sign in the evaluation of suspected acute cholecystitis. J Clin Ultrasound. 1995;23(3):169–72.
Villar J, Summers S, Menchine M, Fox J, Wang R. The absence of gallstones on point-of-care ultrasound rules out acute cholecystitis. J Emerg Med. 2015;49(4):475–80.
Stogryn S, Metcalfe J, Vergis A, Hardy K. Does ultrasongraphy predict intraoperative findings at cholecystectomy? An institutional review. Can J Surg. 2016;59(1):12–8.
Sahani D, Samir A. Abdominal imaging, 2nd ed. Elsevier 2017. Chapter 56: Diffuse Gallbladder Wall Thickening; pp 609-627.
Smith E, Dillman J, Elsayes K, Menias C, Bude R. Cross-sectional imaging of acute and chronic gallbladder inflammatory disease. Am J Roentgenol. 2009;192(1):188–96.
Bolondi L, Gaiani S, Testa S, Labo G. Gall bladder sludge formation during prolonged fasting after gastrointestinal tract surgery. Gut. 1985;26(7):734–8.
Rozycki G, Ballard R, Feliciano D, Schmidt J, Pennington S. Surgeon-performed ultrasound for the assessment of truncal injuries. Ann Surg. 1998;228(4):557–67.
Brooks A. Emergency ultrasound in the acute assessment of haemothorax. Emerg Med J. 2004;21(1):44–6.
Scruggs W, Fox P, Potts B, Zidenny A, McDonough J, Anderson C et al. Accuracy of ED Bedside Ultrasound for Identification of gallstones: retrospective analysis of 575 studies. West J Emerg Med [Internet]. 2008. [cited 22 December 2018];9(2):129. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672232/.
Gaspari R, Dickman E, Blehar D. Learning curve of bedside ultrasound of the gallbladder. J Emerg Med. 2009;37(1):51–6.
Kameda T, Taniguchi N. Overview of point-of-care abdominal ultrasound in emergency and critical care. J Intensive Care. 2016;4:1.
Concannon E, McHugh S, Healy D, Kavanagh E, Burke P, Clarke Moloney M, et al. Diagnostic accuracy of non-radiologist performed ultrasound for abdominal aortic aneurysm: systematic review and meta-analysis. Int J Clin Pract. 2014;68(9):1122–9.
Beggs A, Thomas P. Point of use ultrasound by general surgeons: review of the literature and suggestions for future practice. Int J Surg. 2013;11(1):12–7.
Limchareon S, Jaidee W. Physician-performed focused ultrasound: an update on its role and performance. J Med Ultrasound. 2015;23(2):67–70.
Arhami Dolatabadi A, Amini A, Hatamabadi H, Mohammadi P, Faghihi-Kashani S, Derakhshanfar H, et al. Comparison of the accuracy and reproducibility of focused abdominal sonography for trauma performed by emergency medicine and radiology residents. Ultrasound Med Biol. 2014;40(7):1476–82.
Cazes N, Desmots F, Geffroy Y, Renard A, Leyral J, Chaumoître K. Emergency ultrasound: a prospective study on sufficient adequate training for military doctors. Diagnost Interventional Imaging. 2013;94(11):1109–15.
Summers S, Scruggs W, Menchine M, Lahham S, Anderson C, Amr O, et al. A prospective evaluation of emergency department bedside ultrasonography for the detection of acute cholecystitis. Ann Emerg Med. 2010;56(2):114–22.
Rosen C, Brown D, Chang Y, Moore C, Averill N, Arkoff L, et al. Ultrasonography by emergency physicians in patients with suspected cholecystitis. Am J Emerg Med. 2001;19(1):32–6.
Hilsden R, Leeper R, Koichopolos J, Vandelinde J, Parry N, Thompson D, et al. Point-of-care biliary ultrasound in the emergency department (BUSED): implications for surgical referral and emergency department wait times. Trauma Surg Acute Care Open. 2018;3(1):e000164.
Ross M, Brown M, McLaughlin K, Atkinson P, Thompson J, Powelson S, et al. Emergency physician-performed ultrasound to diagnose cholelithiasis: a systematic review. Acad Emerg Med. 2011;18(3):227–35.
Kendall J, Shimp R. Performance and interpretation of focused right upper quadrant ultrasound by emergency physicians. J Emerg Med. 2001;21(1):7–13.
American College of Emergency Physicians [Internet]. Acep.org. 2018. https://www.acep.org/#sm.0000182s8wudfzey9vfhxife4vjwr. Accessed 22 Dec 2018.
Jang T, Aubin C, Naunheim R. Minimum training for right upper quadrant ultrasonography. Am J Emerg Med. 2004;22(6):439–43.
Ćwik G, Skoczylas T, Wyroślak-Najs J, Wallner G. The value of percutaneous ultrasound in predicting conversion from laparoscopic to open cholecystectomy due to acute cholecystitis. Surg Endosc. 2013;27(7):2561–8.
Siddiqui M, Rizvi S, Sartaj S, Ahmad I, Rizvi S. A standardized ultrasound scoring system for preoperative prediction of difficult laparoscopic cholecystectomy. J Med Ultrasound. 2017;25(4):227–31.
Sutcliffe R, Hollyman M, Hodson J, Bonney G, Vohra R, Griffiths E, et al. Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective UK database of 8820 patients. HPB. 2016;18(11):922–8.
Augustine A, Rao R, Vivek M. A comprehensive predictive scoring method for difficult laparoscopic cholecystectomy. J Minimal Access Surg. 2014;10(2):62.
Bouassida M, Chtourou M, Charrada H, Zribi S, Hamzaoui L, Mighri M, et al. The severity grading of acute cholecystitis following the Tokyo Guidelines is the most powerful predictive factor for conversion from laparoscopic cholecystectomy to open cholecystectomy. J Visc Surg. 2017;154(4):239–43.
Carmody E, Arenson A, Hanna S. Failed or difficult laparoscopic cholecystectomy: can preoperative ultrasonography identify potential problems? J Clin Ultrasound. 1994;22(6):391–6.
Gurusamy K, Rossi M, Davidson B. Percutaneous cholecystostomy for high-risk surgical patients with acute calculous cholecystitis. Cochrane Datab Syst Rev. 2013;2013:8.
Mauro M, Venbrux A, Murphy K, Thomson K, Morgan R. Image-Guided Interventions: Expert Radiology Series (Expert Consult - Online and Print). 2nd ed. Elsevier Health Sciences; 2014. Chapter 137, Percutaneous Coholecystostomy; 1008-1013.
Mahnken A, Wilhelm K, Ricke J. CT- and MR-guided interventions in radiology. Berlin: Springer; 2013.
Mori Y, Itoi T, Baron T, Takada T, Strasberg S, Pitt H, et al. Tokyo Guidelines 2018: management strategies for gallbladder drainage in patients with acute cholecystitis (with videos). J Hepato-Biliary-Pancreat Sci. 2017;25(1):87–95.
Lin W, Chang C, Chu C. Percutaneous cholecystostomy for acute cholecystitis in high-risk elderly patients. Kaohsiung J Med Sci. 2016;32(10):518–25.
Kortram K, van Ramshorst B, Bollen T, Besselink M, Gouma D, Karsten T, et al. Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy (CHOCOLATE trial): Study protocol for a randomized controlled trial. Trials. 2012;13:1.
Gulaya K, Desai S, Sato K. Percutaneous cholecystostomy: evidence-based current clinical practice. Semin Interventional Radiol. 2016;33(04):291–6.
Granlund A, Karlson B, Elvin A, Rasmussen I. Ultrasound-guided percutaneous cholecystostomy in high-risk surgical patients. Langenbeck’s Arch Surg. 2001;386(3):212–7.
Vilaverde F, Sousa M, Mesquita R, Pinto J, Reis A. US-GUIDED Cholecystectomy: a retrospective study of indications, complications and outcome. Acta Radiol Portuguesa. 2015;27(104):17–20.
Eggermont A. Ultrasound-Guided percutaneous transhepatic cholecystostomy for acute acalculous cholecystitis. Arch Surg. 1985;120(12):1354.
Requarth J. Ultrasound-guided percutaneous cholecystostomy in pregnancy. J Am Coll Surg. 2010;211(1):145.
Allmendinger N, Hallisey M, Ohki S, Johnstraub J. Percutaneous cholecystostomy treatment of acute cholecystitis in pregnancy. Obstet Gynecol. 1995;86(4):653–4.
Dewhurst C, Kane R, Mhuircheartaigh J, Brook O, Sun M, Siewert B. Complication rate of ultrasound-guided percutaneous cholecystostomy in patients with coagulopathy. Am J Roentgenol. 2012;199(6):W753–60.
Başaran O, Yavuzer N, Selçuk H, Harman A, Karakayali H, Bilgin N. Ultrasound-guided percutaneous cholecystostomy for acute cholecystitis in critically ill patients: one center’s experience. Turk J Gastroenterol. 2005;3(16):134–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state to have no conflict of interest regarding this manuscript.
Additional information
Consensus Conference: European Congress for Trauma & Emergency Surgery, Palais de Congressos, Valencia, Spain, 6th May 2018.
Rights and permissions
About this article
Cite this article
Pereira, J., Bass, G.A., Mariani, D. et al. Surgeon-performed point-of-care ultrasound for acute cholecystitis: indications and limitations: a European Society for Trauma and Emergency Surgery (ESTES) consensus statement. Eur J Trauma Emerg Surg 46, 173–183 (2020). https://doi.org/10.1007/s00068-019-01197-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01197-z