Abstract
Purpose
Olecranon fractures are common and typically require surgical fixation due to displacement generated by the pull of the triceps muscle. The most common techniques for repairing olecranon fractures are tension-band wiring or plate fixation, but these methods are associated with high rates of implant-related soft-tissue irritation. Another treatment option is fixation with an intramedullary screw, but less is known about surgical results using this strategy. Thus, the purpose of this study was to report the clinical and functional outcomes of olecranon fractures treated with an intramedullary cannulated screw.
Methods
We identified 15 patients (average age at index procedure 44 years, range 16–83) with a Mayo type I or IIA olecranon fracture who were treated with an intramedullary cannulated screw at a single level 2 trauma center between 2012 and 2017. The medical record was reviewed to assess radiographic union, postoperative range of motion and complications (including hardware removal). Patient-reported outcome was evaluated using the Disabilities of the Arm, Shoulder and Hand (DASH) score. Average follow-up was 22 months (range 8–36 months).
Results
By the 6th month post-operative visit, 14 patients had complete union of their fracture and 1 patient had an asymptomatic non-union that did not require further intervention. Average flexion was 145° (range 135–160) and the average extension lag was 11° (range 0–30). Implants were removed in 5 patients due to soft-tissue irritation. Average DASH score (± standard deviation) by final follow-up was 16 ± 10.
Conclusions
Fixation of simple olecranon fractures with an intramedullary screw is a safe and easy fixation method in young patients, leading to good functional and radiological results. Compared to available data, less hardware removal is necessary than with tension-band wiring or plate fixation.
Similar content being viewed by others
Introduction
Olecranon fractures are relatively common injuries and account for approximately 10% of upper extremity fractures in adults [1]. Traction of the triceps on the proximal fragment often leads to disruption of articular congruity and of the elbow’s extension mechanism. As a result, this injury is typically treated with open reduction and internal fixation (ORIF) [1,2,3,4,5]. Common techniques to treat simple olecranon fractures are tension-band wiring and plate fixation [1,2,3,4,5,6,7,8,9,10,11]. As the skin is thin at the proximal ulna with relatively little subcutaneous tissue, these fixation methods often lead to implant-related soft-tissue irritation necessitating implant removal in 68–82% of the cases largely based on the fixation method that was used [3,4,5, 12].
While intramedullary screw fixation is commonly used to fix olecranon osteotomies [13, 14] fewer reports have been published on its use for simple (Mayo type I or IIA) olecranon fractures (Fig. 1). Successful fixation with an intramedullary screw was first described in 1942 by MacAusland, but subsequent reports noted that the technique was challenging and unreliable [11, 15,16,17,18].
However, many of these studies are older without clear inclusion criteria or CT imaging. As we have learned more about the morphology of the ulna and proximal ulna fractures [19,20,21], it is less clear if early reports about the unreliability of intramedullary screw fixation were related solely to implant choice or to the use of an intramedullary screw for inappropriate (i.e., more complex) fracture types [22]. Thus, the purpose of this study was to assess the clinical and functional outcomes of simple olecranon fractures treated with an intramedullary cannulated screw.
Methods
Study design and inclusion criteria
For this retrospective study, we used billing records of a single level 2 trauma center to identify patients with a proximal ulna fracture treated between June 2014 and June 2017. The medical records and radiology images of these patients were reviewed: extra-articular ulna fractures, combined forearm fractures, comminuted olecranon fractures and all patients treated conservatively or with tension-band wiring or plate fixation were excluded. Based on these restrictions, we identified 15 patients (age > 16 years) with a Mayo type I or IIA olecranon fracture that was treated with an intramedullary 7.3 mm cannulated screw.
Surgical technique
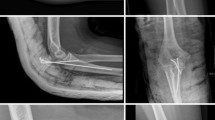
The patient is placed in the supine position with the arm draped over the chest. A straight posterior incision is made from the tip of the olecranon to 1 cm distal of the fracture. The fracture is irrigated and then reduced anatomically. Provisional fixation is obtained with two parallel bicortical 1.0 mm k-wires that are placed in such a way that they will not hinder the placement of the 7.3 cannulated intramedullary screw (Fig. 2a, b). We use two k-wires for provisional fixation to prevent rotation of the proximal ulna during placement of the screw. A small longitudinal incision is made at the triceps insertion over the centre–centre point of the palpable olecranon tip to facilitate placement of an intramedullary 2.8 mm guide wire (Fig. 2c, d) [23]. Screw length is then measured such that the distal threaded end of the screw will engage the narrow marrow of the proximal ulnar diaphysis (typically 90–110 mm) to provide stable fixation. The cortex is opened with the cannulated drill and the screw is placed. Depending on surgeon preference, an additional washer can be used (Fig. 2e). The guidewire and the two anti-rotation k-wires are then removed (Fig. 2f).
Overview of intra-operative fluoroscopy imaging: temporary reduction with bicortical anti-rotation k-wires (a, b). intramedullary placement of guide wire centre–centre on the olecranon tip into the ulnar shaft (c, d). Placement of the partially threaded cannulated screw over the guide wire (e). Final imaging after removal of the guidewire and the anti-rotation k-wires (f)
Postoperative management and follow-up
The arm is placed in a padded bulky dressing for the first 24 h. All patients are allowed full active and passive range of motion, but are limited to non-weightbearing activities for the first 6 weeks. Patients are then seen at the outpatient clinic at regular intervals (2, 6, 12 and 24 weeks) until radiographic healing is observed.
Evaluation
We recorded radiographic union, postoperative range of motion and complications (including hardware removal). Radiographic union was based on the most recently available radiograph. Active range of motion and implant-related complaints were noted in the electronic medical record. Patient-reported outcome was evaluated using the Disabilities of the Arm, Shoulder and Hand (DASH) score (including the Sport and Work sections) [24]. In general, the DASH ranges from 0 (no disability) to 100 (most severe disability), with lower scores denoting better function. In this study, we used the Dutch version of the DASH. We also assessed operating time as a proxy for procedure complexity.
Statistical analysis
Data were collected in a Microsoft Excel 2016 database. Descriptive statistics were calculated for demographic characteristics, range of motion, complications, and patient-reported outcome (DASH). This study was approved by our Institutional Review Board.
Results
Study population
We identified 15 patients with a simple olecranon fracture (Mayo IA/IIA) that was treated with a 7.3 mm cannulated intramedullary screw. Fourteen of the 15 fractures were displaced (Mayo IIA) and 1 fracture was slightly displaced (Mayo IA). Average age of these patients was 44 years (range 16–83) years (Tables 1, 2). Ten patients were ASA I, 4 were ASAII and 1 patient was ASA III at their pre-operative screening. A washer was used in 10 patients, while 5 patients were treated with just a screw. Average duration operative time was 46 min (median = 41 min; range 35–72 min).
Surgical results
The majority (14 out of 15) of fractures treated with intramedullary screw demonstrated healing by the time of final follow-up. One patient developed an asymptomatic non-union and another patient had an asymptomatic malunion; both were the oldest patients in the cohort and did not require any surgical intervention (Table 2). None of the patients required revision surgery. Average flexion was 145 ± 10°, average extension was 11 ± 6°, and average active range of motion was 134 ± 16° (Table 3; Fig. 3). Except for the patient with a non-union, all patients had at least 30° extension, 130° flexion, and at least a 100° flexion–extension arc (Table 3).
Complications
Other than complications related to radiographic healing, the only complication observed in this series was removal of implants due to implant-associated soft-tissue irritation in 5 patients. Interestingly, 4 out of 10 patients treated with a washer required implant removal, while only 1 out of 5 patients treated with screw only required removal. The average time ± SD to hardware removal was 332 ± 206 days.
Patient-reported outcome
DASH scores were available for 12 out of 15 patients (80% response rate). Average DASH scores were 16 ± 10. Average scores on the DASH work module were 7 ± 10, while average scores on the DASH sports module were 27 ± 20 (Table 2).
Discussion
While tension-band wiring and ORIF with plate fixation are both effective treatments for olecranon fractures, we propose that fixation of simple olecranon fractures using an intramedullary screw is also a reasonable option based on the results of this series. Previous studies have suggested that fixation using intramedullary cannulated screws is technically challenging and unreliable [11, 15,16,17,18], but we found that this technique lead to acceptable surgical results, good patient-reported outcomes, and low rates of implant removal with reasonable operative times (average 45 min).
When surgical treatment is indicated, several treatment options, such as tension-band wiring, plate fixation, intramedullary screw fixation and intramedullary nail fixation have been described [1,2,3,4,5, 7,8,9,10,11]. These techniques differ in their method of fixation and have their own advantages and disadvantages, but a recent Cochrane review found that none was definitively preferable based on available evidence [2]. Tension-band wiring has shown excellent results with regard to union rates [2, 3, 9] and remains the first choice of treatment for many due to the low complexity and costs of the [8, 9]. Yet, implant removal is often necessary due to hardware irritation or k-wire migration in up to 82% of patients [3, 7]. Another technique often used is plate fixation [5, 8, 9, 25]. This technique is especially indicated in comminuted fractures and with osteoporotic bone, but can also be used for simple two-part fractures [5, 8]. In a recent prospective trial comparing plate fixation and tension-band wiring, there was no difference in union, DASH, function or costs, and plate fixation was associated with a decreased rate of implant removal [3]. However, this was offset by the increased number of infections and revisions in the plate fixation group [3]. Since neither of these options is optimal for all settings, we propose that intramedullary screw fixation should also be considered for simple olecranon fractures based on our results.
Many reasons exist for differences between our study and existing literature [11, 15,16,17]. The prior studies are small and often include a wide variety of fractures treated with intramedullary screws, and frequently in settings where plate fixation would have been more appropriate given our greater understanding of proximal ulna fracture morphology [19,20,21]. For example, in the series published by Helm et al., 79% of treated fractures were comminuted [17]. In the present day, with more accurate radiologic diagnostics including improved X-rays and CT scans, identifying appropriate cases (e.g., simple olecranon fractures) is easier and likely to lead to better outcomes [22]. Moreover, using intramedullary screw fixation for simple Mayo type 1 and 2A fractures is somewhat intuitive since these fracture types are most similar to olecranon osteotomies which are known to heal well with screw fixation. And in many cases, use of a screw instead of tension-band wiring also led to decreased rates of implant removal [18].
Except for one elderly frail patient with an asymptomatic non-union, all patients healed their fracture. Mechanically, the partially threaded intramedullary screw works as a lag-screw. When inserted across the fracture, the threads of the screw tip engage in the cancellous bone of the metaphyseal area, causing compression of the fracture fragments upon tightening. In osteoporotic bone the screw may not have enough purchase for a stable fixation and the proximal part may be pulled away by the force of the triceps muscle. In our series, both the malunion and the non-union patient were geriatric patients with osteoporotic bone (Table 2). Based on these results, this fixation method may not be suitable for this patient group although this requires further study.
A prior study demonstrated that the dominant factor driving re-operation for isolated olecranon fractures was the type of fixation. In that study, tension-band wiring had over twice the rate of implant removal as ORIF using plates (46.5% vs. 18.7%, respectively), and rates using intramedullary implants were not studied [12]. Based on our results, intramedullary screw fixation has rates of removal that are in-between these two fixation methods. Other, earlier studies [3,4,5] have shown higher removal rates for tension-band wiring and plate fixation up to 68–82%. In addition, we did not observe any superficial or deep infections and this may have been due to the fact that, compared to tension-band wiring or plate fixation, a smaller incision could be used with minimal soft-tissue dissection or trauma. However, further studies with larger number of patients comparing between fixation options are needed to better answer these questions.
Finally, during the last 20 years several intramedullary nails have been described [10, 26, 27]. The nails have the same advantage as the intramedullary screw as they are low profile and have almost no protruding hardware. However, intramedullary nails are more complex and often designed for use with more complex fractures. For simple Mayo IA or 2A fractures, these extra design features are likely not necessary and simple screw fixation is likely to be sufficient and probably less expensive. We did not observe complications related to the insertion of a straight rigid intramedullary screw into a bone with a complex curved morphology. We believe this is because the varus curvature of the proximal ulna begins at approximately 8.2 cm from the olecranon tip and the anterior angulation starts at approximately 8.6 cm, while the inserted screws were only between 9 and 10 cm [28]. These anatomic characteristics highlight the importance of the central–central insertion point in facilitating the optimal direction of the screw [23].
Limitations of study
This study has several limitations. As this was not a prospective randomized control trial, patient selection may be biased by the preference of the treating surgeons. However, our goal was to illustrate that this well-described technique may be more reliable than previously suggested. We had 100% follow-up rate for clinical exam and a 80% response rate to the DASH survey which minimized response bias. Finally, we studied a relatively small number of patients making it difficult to make robust statistical comparisons. However, given that this is an uncommon technique which we used for very specific indications, these results may help support the use of intramedullary screws at other institutions to allow for larger studies.
Conclusion
Fixation of simple olecranon fractures using an intramedullary screw is a reasonable option, leading to acceptable surgical results, good patient-reported outcomes, and low rates of implant removal. Future work is needed to compare outcomes against other fixation options and to study other possible indications for its use.
Change history
25 November 2019
The original version of this article unfortunately contained some mistakes. The spelling of the Willem Maarten P. F. Bosmans’ name was incorrect.
References
Wiegand L, Bernstein J, Ahn J. Fractures in brief: olecranon fractures. Clin Orthop Relat Res. 2012;470:3637–41.
Matar HE, Ali AA, Buckley S, Garlick NI, Atkinson HD. Surgical interventions for treating fractures of the olecranon in adults. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD010144.pub2.
Duckworth AD, Clement ND, White TO, Court-Brown CM, McQueen MM. Plate versus tension-band wire fixation for olecranon fractures: a prospective randomized trial. J Bone Jt Surg Am. 2017;99:1261–73.
Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. 2012;43:343–6.
Nork SE, Jones CB, Henley MB. Surgical treatment of olecranon fractures. Am J Orthop. 2001;30:577–86.
Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000;8:266–75.
Newman SDS, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40:575–81.
Wood T, Thomas K, Farrokhyar F, Ristevski B, Bhandari M, Petrisor B. A survey of current practices and preferences for internal fixation of displaced olecranon fractures. Can J Surg. 2015;58:250–6.
Hamer den A, Heusinkveld M, Traa W, Oomen P, Oliva F, Del Buono A, et al. Current techniques for management of transverse displaced olecranon fractures. Muscles Ligaments Tendons J. 2015;5:129–40.
Gehr J, Friedl W. Intramedullary locking compression nail for the treatment of an olecranon fracture. Oper Orthop Traumatol. 2006;18:199–213.
Macausland WR. The treatment of fractures of the olecranon by longitudinal screw or nail fixation. Ann Surg. 1942;116:293–6.
Snoddy MC, Lang MF, An TJ, Mitchell PM, Grantham WJ, Hooe BS, et al. Olecranon fractures: factors influencing re-operation. Int Orthop. 2014;38:1711–6.
Coles CP, Barei DP, Nork SE, Taitsman LA, Hanel DP, Bradford Henley M. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma. 2006;20:164–71.
Woods BI, Rosario BL, Siska PA, Gruen GS, Tarkin IS, Evans AR. Determining the efficacy of screw and washer fixation as a method for securing olecranon osteotomies used in the surgical management of intraarticular distal humerus fractures. J Orthop Trauma. 2015;29:44–9.
Colton CL. Fractures of the olecranon in adults: classification and management. Injury. 1973;5:121–9.
Wadsworth TG. Screw fixation of the olecranon. Lancet. 1976;2:1118–9.
Helm RH, Hornby R, Miller SW. The complications of surgical treatment of displaced fractures of the olecranon. Injury. 1987;18:48–50.
Ahmed AR, Sweed T, Wanas A. The role of cancellous screw with tension band fixation in the treatment of displaced olecranon fractures, a comparative study. Eur J Orthop Surg Traumatol. (3rd ed). 2008;18:571–6.
Fujihara Y, Tatebe M, Fujihara N, Tanaka H, Hirata H. Morphological characteristics of olecranon fractures in adults: a computed tomography-based study. Acta Orthop Belg. 2016;82:313–8.
Chapleau J, Balg F, Harvey EJ, Ménard J, Vauclair F, Laflamme G-Y, et al. Impact of olecranon fracture malunion: study on the importance of PUDA (proximal ulna dorsal angulation). Injury. 2016;47:2520–4.
Kachooei AR, Mellema JJ, Tarabochia MA, Chen N, van Dijk CN, Ring D. Involvement of the lesser sigmoid notch in elbow fracture dislocations. J Shoulder Elbow Surg. 2016;25:1571–6.
Morwood MP, Ruch DS, Leversedge FJ, Mithani SK, Kamal RN, Richard MJ. Olecranon fractures with sagittal splits treated with dual fixation. J Hand Surg. 2015;40:711–5.
Potter GD, Mascarenhas D, Sciadini MF, Carlini AR, O’Toole RV, Pensy RA. What is the ideal starting point for an olecranon screw? An anatomic cadaveric study. J Orthop Trauma. 2018;32:1–319.
Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29(6):602–8.
Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Jt Surg Am. 2009;91:2416–20.
Argintar E, Cohen M, Eglseder A, Edwards S. Clinical results of olecranon fractures treated with multiplanar locked intramedullary nailing. J Orthop Trauma. 2013;27:140–4.
Edwards SG, Argintar E, Lamb J. Management of comminuted proximal ulna fracture-dislocations using a multiplanar locking intramedullary nail. Tech Hand Up Extrem Surg. 2011;15:106–14.
Totlis T, Anastasopoulos N, Apostolidis S, Paraskevas G, Terzidis I, Natsis K. Proximal ulna morphometry: which are the “true” anatomical preshaped olecranon plates? Surg Radiol Anat. 2014;36:1015–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Willem-Maarten Bosman declares that he has no conflict of interest. Benjamin Emmink declares that he has no conflict of interest. Marijn Houwert declares that he has no conflict of interest. Abhiram Bhashyam declares that he has no conflict of interest. Jort Keizer declares that he has no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bosman, WM.P.F., Emmink, B.L., Bhashyam, A.R. et al. Intramedullary screw fixation for simple displaced olecranon fractures. Eur J Trauma Emerg Surg 46, 83–89 (2020). https://doi.org/10.1007/s00068-019-01114-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01114-4