Abstract
Purpose
The risk of developing acute radiotherapy(RT)-induced side effects may increase with hypofractionated RT. To detect treatment-related side effects, patient-reported outcomes (PROs) might be more reliable than physician-reported outcomes. Therefore, we tried to evaluate the rate of agreement between urinary and gastrointestinal (GI) side effects and the prevalence of side effects reported by patients and by physicians.
Methods
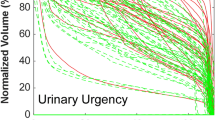
Data from a randomized controlled trial (RCT) comparing two hypofractionated RT schedules were used. Urinary (nocturia, incontinence, frequency, dysuria, and urgency) and GI (obstruction, diarrhea, vomiting, nausea, bloating, hemorragia, and incontinence) symptoms measured by the EORTC QLQ-C30 and PR-25 were used for PROs. The same symptoms were scored by the physician using the Common Terminology Criteria Adverse Events v4.0. Outcomes were reported at baseline, end of treatment, month 1, and month 3. PROs and physician-reported outcomes were converted in two categories (0 = no symptoms; 1 = symptoms of any severity) and were correlated using the kappa (κ) correlation statistics. Values below 0.40 were considered low agreement. In addition, the prevalence of symptoms was calculated.
Results
Data from 160 patients were used. The mean value for Cohen’s κ was 0.31 (ranging between 0.04 and 0.55) and 0.23 (ranging between 0.04 and 0.47) for urinary and GI symptoms, respectively. Except for three symptoms at baseline, all symptoms reported by patients were higher than those reported by physicians.
Conclusion
There is low agreement between symptoms reported by patients and physicians, with high rates of underreporting by the physician.
Zusammenfassung
Zielsetzung
Das Risiko des Entstehens von akuten Strahlentherapie(RT)-induzierten Nebenwirkungen erhöht sich bei hypofraktionierter Bestrahlung. Um behandlungsbedingte Nebenwirkungen aufzudecken, könnten von Patienten berichtete Ergebnisse (PRO) verlässlicher sein als die vom Arzt. Wir wollen daher die Übereinstimmungsrate zwischen Harnwegsnebenwirkungen und gastrointestinalen (GI) Nebenwirkungen und der Prävalenz der von Patienten und Ärzten berichteten Nebenwirkungen beurteilen.
Methoden
Verwendet wurden Daten aus einer randomisierten, kontrollierten Studie (RCT), in der zwei hypofraktionierte Bestrahlungsschemata verglichen wurden. Für die Beurteilung der PRO wurden Harnwegs- (Nykturie, Inkontinenz, häufiges Wasserlassen, Dysurie und Harndrang) und GI-Symptome (Verstopfung, Durchfall, Erbrechen, Übelkeit, Blähungen, Blutungen und Stuhlinkontinenz) anhand der QLQ-C30- und PR-25-Fragebögen der EORTC (European Organisation for Research and Treatment of Cancer) gemessen. Die gleichen Symptome wurden vom Arzt anhand des Common Terminology Criteria Adverse Events v4.0 bewertet. Die Ergebnisse wurden bei Baseline, Behandlungsende und nach Monat 1 und Monat 3 berichtet. PRO und vom Arzt berichtete Ergebnisse wurden in zwei Kategorien überführt (0 = keine Symptome, 1 = Symptome jeglicher Schwere) und mithilfe der Kappa(κ)-Statistik nach Cohen miteinander korreliert. Werte von weniger als 0,40 wurden als geringe Übereinstimmung angesehen. Außerdem wurde die Prävalenz der Symptome berechnet.
Ergebnisse
Verwendet wurden Daten von 160 Patienten. Der mittlere Cohen-κ-Wert betrug 0,31 (bei Werten zwischen 0,04 und 0,55) für Harnwegssymptome und 0,23 (bei Werten zwischen 0,04 und 0,47) für GI-Symptome. Mit Ausnahme von drei Symptomen bei Baseline waren alle patientenberichteten Symptome höher bewertet als die der Ärzte.
Schlussfolgerung
Zwischen den von Patienten und von Ärzten berichteten Symptomen besteht eine geringe Übereinstimmung, mit hohen Untererfassungsraten („underreporting“) durch die Ärzte.


Similar content being viewed by others
References
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71(4):618–629
Thames HD, Withers HR, Peters LJ, Fletcher GH (1982) Changes in early and late radiation responses with altered dose fractionation: implications for dose-survival relationships. Int J Radiat Oncol Biol Phys 8(2):219–226
Vogelius IR, Bentzen SM (2013) Meta-analysis of the alpha/beta ratio for prostate cancer in the presence of an overall time factor: bad news, good news, or no news? Int J Radiat Oncol Biol Phys 85(1):89–94
Zemplényi A, Kaló Z, Kovács G, Farkas R, Beöthe T, Bányai D et al (2016) Cost-effectiveness analysis of intensity-modulated radiation therapy with normal and hypofractionated schemes for the treatment of localised prostate cancer. Eur J Cancer Care (Engl). https://doi.org/10.1111/ecc.12430
Dearnaley D, Syndikus I, Sumo G, Bidmead M, Bloomfield D, Clark C et al (2012) Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: preliminary safety results from the CHHiP randomised controlled trial. Lancet Oncol 13(1):43–54
Catton CN, Lukka H, Gu C‑S, Martin JM, Supiot S, Chung PW et al (2017) Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol. https://doi.org/10.1200/jco.2016.71.7397
Lee WR, Dignam JJ, Amin MB, Bruner DW, Low D, Swanson GP et al (2016) Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol 34(20):2325–2332
Arcangeli G, Saracino B, Arcangeli S, Gomellini S, Petrongari MG, Sanguineti G et al (2017) Moderate hypofractionation in high-risk, organ-confined prostate cancer: final results of a phase III randomized trial. J Clin Oncol. https://doi.org/10.1200/jco.2016.70.4189
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D et al (2016) Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5‑year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 17(8):1047–1060. https://doi.org/10.1016/s1470-2045(16)30102-4
Flores LT, Bennett AV, Law EB, Hajj C, Griffith MP, Goodman KA (2012) Patient-reported outcomes vs. clinician symptom reporting during chemoradiation for rectal cancer. Gastrointest Cancer Res 5(4):119
Di Maio M, Gallo C, Leighl NB, Piccirillo MC, Daniele G, Nuzzo F et al (2015) Symptomatic toxicities experienced during anticancer treatment: agreement between patient and physician reporting in three randomized trials. J Clin Oncol 33(8):910–915
Fromme EK, Eilers KM, Mori M, Hsieh Y‑C, Beer TM (2004) How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. J Clin Oncol 22(17):3485–3490
Aluwini S, Pos F, Schimmel E, van Lin E, Krol S, van der Toorn PP et al (2015) Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): acute toxicity results from a randomised non-inferiority phase 3 trial. Lancet Oncol 16(3):274–283
Wilkins A, Mossop H, Syndikus I, Khoo V, Bloomfield D, Parker C et al (2015) Hypofractionated radiotherapy versus conventionally fractionated radiotherapy for patients with intermediate-risk localised prostate cancer: 2‑year patient-reported outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 16(16):1605–1616
Norkus D, Karklelyte A, Engels B, Versmessen H, Griskevicius R, De Ridder M et al (2013) A randomized hypofractionation dose escalation trial for high risk prostate cancer patients: interim analysis of acute toxicity and quality of life in 124 patients. Radiat Oncol 8:206. https://doi.org/10.1186/1748-717x-8-206
Fonteyne V, Sarrazyn C, Swimberghe M, De Meerleer G, Rammant E, Vanderstraeten B et al (2018) Four-weeks versus 5‑weeks hypofractionated high dose radiotherapy as primary therapy for prostate cancer: interim safety analysis of a randomized phase 3 trial. Int J Radiat Oncol Biol Phys. https://doi.org/10.1016/j.ijrobp.2017.12.016
Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD et al (2013) Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA 309(8):814–822
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
van Andel G, Bottomley A, Fosså SD, Efficace F, Coens C, Guerif S et al (2008) An international field study of the EORTC QLQ-PR25: a questionnaire for assessing the health-related quality of life of patients with prostate cancer. Eur J Cancer 44(16):2418–2424
Fleiss JL, Levin B, Paik MC (2013) Statistical methods for rates and proportions. John Wiley & Sons, New Jersey
Geinitz H, Zimmermann FB, Thamm R, Erber C, Müller T, Keller M et al (2006) Late rectal symptoms and quality of life after conformal radiation therapy for prostate cancer. Radiother Oncol 79(3):341–347
Bacon CG, Giovannucci E, Testa M, Glass TA, Kawachi I (2002) The association of treatment-related symptoms with quality-of-life outcomes for localized prostate carcinoma patients. Cancer 94(3):862–871
Bonet M, Cayetano L, Núñez M, Jovell-Fernández E, Aguilar A, Ribas Y (2018) Assessment of acute bowel function after radiotherapy for prostate cancer: Is it accurate enough? Clin Transl Oncol 20(5):576–583
Schaake W, Wiegman EM, de Groot M, van der Laan HP, van der Schans CP, van den Bergh AC et al (2014) The impact of gastrointestinal and genitourinary toxicity on health related quality of life among irradiated prostate cancer patients. Radiother Oncol 110(2):284–290
Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C, Walsh E et al (2016) Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. New Engl J Med 375(15):1425–1437
Barocas DA, Alvarez J, Resnick MJ, Koyama T, Hoffman KE, Tyson MD et al (2017) Association between radiation therapy, surgery, or observation for localized prostate cancer and patient-reported outcomes after 3 years. JAMA 317(11):1126–1140
Basch E, Deal AM, Dueck AC, Scher HI, Kris MG, Hudis C et al (2017) Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. https://doi.org/10.1001/jama.2017.7156
Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P et al (2015) Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol 34(6):557–565
Bennett AV, Jensen RE, Basch E (2012) Electronic patient-reported outcome systems in oncology clinical practice. CA Cancer J Clin 62(5):336–347
Funding
The present study was supported in part by a grant from Stichting tegen kanker, a nonprofit organization. The funders did not have access to the raw data and had no role in the study design, data collection, data analysis or interpretation, or writing of the report. V. Fonteyne is a post-doctorate clinical specialist funded by the Belgian Foundation against Cancer. R. Bultijnck was supported by a PhD fellowship of The Research Foundation—Flanders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Rammant, P. Ost, M. Swimberghe, B. Vanderstraeten, N. Lumen, K. Decaestecker, R. Bultijnck, G. De Meerleer, C. Sarrazyn, R. Colman, and V. Fonteyne declare that they have no competing interests.
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Rammant, E., Ost, P., Swimberghe, M. et al. Patient- versus physician-reported outcomes in prostate cancer patients receiving hypofractionated radiotherapy within a randomized controlled trial. Strahlenther Onkol 195, 393–401 (2019). https://doi.org/10.1007/s00066-018-1395-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1395-y
Keywords
- Quality of life
- Patient-reported outcomes
- Urinary and gastrointestinal toxicity
- Radiotherapy
- Prostate cancer