Abstract
Background
Conventional catheter ablation of cardiac arrhythmias is associated with radiation risks for patients and laboratory personnel. Widespread use of zero-fluoroscopic catheter ablation in clinical routine is limited by safety concerns. This study investigated the feasibility of zero-fluoroscopy catheter ablation using a three-dimensional mapping system and optional catheter contact force technology for an all-comers collective.
Patients and methods
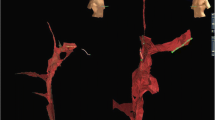
The study comprised 184 patients; 91 patients, including 29 pediatric patients, underwent a zero-fluoroscopic electrophysiology (EP) study using the EnSite NavX system with real-time visualization of all electrodes. These patients were matched to a control group, which was treated using fluoroscopy in the same period. Inclusion criteria were documented supraventricular tachycardia or a history of symptomatic paroxysmal supraventricular tachycardia. Transseptal access, if necessary, was achieved under transesophageal echocardiographic guidance for ablation of left-sided arrhythmias. Radiofrequency (using optional contact force measurement) or a cryotechnique was used for ablation.
Results
We observed no major acute complications. There were no significant differences between the two groups in the follow-up period.
Conclusion
Zero-fluoroscopic catheter ablation is generally feasible in right-sided cardiac arrhythmias. Safety concerns regarding left atrial substrates or children can be overcome with optional real-time contact force measurement.
Zusammenfassung
Hintergrund
Die konventionelle Katheterablation von Herzrhythmusstörungen impliziert sowohl für den Patienten als auch für das behandelnde Katheterpersonal ein relevantes Strahlenschadensrisiko. Der routinemäßige, breite Einsatz einer strahlenfreien Katheterablation ist allerdings wegen Sicherheitsbedenken limitiert. Ziel dieser Studie ist es, die Durchführbarkeit einer strahlenfreien Katheterablation mittels 3-D-Mapping-System und optionaler Anpresskraftkontrolle in einem breiten Patientenkollektiv zu untersuchen.
Patienten und Methoden
184 Patienten wurden in die Studie eingeschlossen. Bei 91 Patienten, inklusive 29 pädiatrischen Patienten, wurde eine strahlenfreie EPU mittels Ensite-NavX-System durchgeführt. Diese Patienten wurden mit einer Kontrollgruppe verglichen, die mittels Durchleuchtung untersucht wurde. Einschlusskriterien waren eine dokumentierte oder anamnestische paroxysmale supraventrikuläre Tachykardie. Ein transseptaler Zugang für linksatriale Ablationen wurde unter TEE-Führung erzielt. Zur Ablationstherapie wurde entweder Radiofrequenz (mit optionaler Anpresskraftkontrolle) oder Kryotechnik eingesetzt.
Ergebnisse
Es trat keine relevante Akutkomplikation auf. Insgesamt wurde kein signifikanter Unterschied in den beiden Gruppen festgestellt.
Schlussfolgerung
Die komplett strahlenfreie Katheterablation ist generell bei rechtsatrialen Rhythmusstörungen möglich. Die Sicherheit kann bei linksatrialen Eingriffen und bei Kindern durch den Einsatz der Anpresskraftkontrolle erhöht werden.



Similar content being viewed by others
References
Clay MA, Campbell RM, Strieper M, Frias PA, Stevens M, Mahle WT (2008) Long-term risk of fatal malignancy following pediatric radiofrequency ablation. Am J Cardiol 102:913–915
Roguin A, Goldstein J, Bar O, Goldstein JA (2013) Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol 111:1368–1372
Roguin A (2012) Brain tumours among interventional cardiologists: a call for alarm? Eur Heart J 33:1850–1851
Ernst S, Castellano I (2013) Radiation exposure and safety for the electrophysiologist. Curr Cardiol Rep 15:402
Fernandez-Gomez JM, Morina-Vazquez P, Morales Edel R, Venegas-Gamero J, Barba-Pichardo R, Carranza MH (2014) Exclusion of fluoroscopy use in catheter ablation procedures: six years of experience at a single center. J Cardiovasc Electrophysiol 25:638–644
Gist K, Tigges C, Smith G, Clark J (2011) Learning curve for zero-fluoroscopy catheter ablation of avnrt: early versus late experience. Pacing Clin Electrophysiol 34:264–268
Alvarez M, Tercedor L, Almansa I, Ros N, Galdeano RS, Burillo F, Santiago P, Penas R (2009) Safety and feasibility of catheter ablation for atrioventricular nodal re-entrant tachycardia without fluoroscopic guidance. Heart Rhythm 6:1714–1720
Tuzcu V (2007) A nonfluoroscopic approach for electrophysiology and catheter ablation procedures using a three-dimensional navigation system. Pacing Clin Electrophysiol 30:519–525
Earley MJ, Showkathali R, Alzetani M, Kistler PM, Gupta D, Abrams DJ, Horrocks JA, Harris SJ, Sporton SC, Schilling RJ (2006) Radiofrequency ablation of arrhythmias guided by non-fluoroscopic catheter location: a prospective randomized trial. European heart journal 27:1223–1229
Clark J, Bockoven JR Lane J, Patel CR, Patel CR, Smith G (2008) Use of three-dimensional catheter guidance and trans-esophageal echocardiography to eliminate fluoroscopy in catheter ablation of left-sided accessory pathways. Pacing Clin Electrophysiol 31:7
Reddy VY, Morales G, Ahmed H, Neuzil P, Dukkipati S, Kim S, Clemens J, D'Avila A (2010) Catheter ablation of atrial fibrillation without the use of fluoroscopy. Heart Rhythm 7:1644–1653
Ferguson JD, Helms A, Mangrum JM, Mahapatra S, Mason P, Bilchick K, McDaniel G, Wiggins D, DiMarco JP (2009) Catheter ablation of atrial fibrillation without fluoroscopy using intracardiac echocardiography and electroanatomic mapping. Circ Arrhythm Electrophysiol 2:611–619
Kuck KH, Reddy VY, Schmidt B, Natale A, Neuzil P, Saoudi N, Kautzner J, Herrera C, Hindricks G, Jais P, Nakagawa H, Lambert H, Shah DC (2012) A novel radiofrequency ablation catheter using contact force sensing: Toccata study. Heart Rhythm 9:18–23
Kerst G, Weig HJ, Weretka S, Seizer P, Hofbeck M, Gawaz M, Schreieck J (2012) Contact force-controlled zero-fluoroscopy catheter ablation of right-sided and left atrial arrhythmia substrates. Heart Rhythm 9:709–714
Hindricks G, Willems S, Kautzner J, De Chillou C, Wiedemann M, Schepel S, Piorkowski C, Risius T, Kottkamp H, EuroFlutter I (2009) Effect of electroanatomically guided versus conventional catheter ablation of typical atrial flutter on the fluoroscopy time and resource use: a prospective randomized multicenter study. J Cardiovasc Electrophysiol 20:734–740
Macias R, Uribe I, Tercedor L, Jimenez J, Barrio T, Alvarez M (2014) A zero-fluoroscopy approach to cavotricuspid isthmus catheter ablation: comparative analysis of two electroanatomical mapping systems. Pacing Clin Electrophysiol 37:1029–1037
Papagiannis J, Tsoutsinos A, Kirvassilis G, Sofianidou I, Koussi T, Laskari C, Kiaffas M, Apostolopoulou S, Rammos S (2006) Nonfluoroscopic catheter navigation for radiofrequency catheter ablation of supraventricular tachycardia in children. Pacing Clin Electrophysiol 29:971–978
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Seizer, V. Bucher, C. Frische, D. Heinzmann, M. Gramlich, I. Müller, A. Henning, M. Hofbeck, G. Kerst, M. Gawaz, and J. Schreieck state that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Seizer, P., Bucher, V., Frische, C. et al. Efficacy and safety of zero-fluoroscopy ablation for supraventricular tachycardias. Herz 41, 241–245 (2016). https://doi.org/10.1007/s00059-015-4358-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-015-4358-4