Abstract
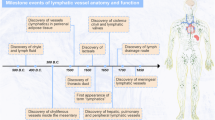
Hippocratic Corpus, a collection of Greek medical literature, described the functional anatomy of the lymphatic system in the fifth century B.C. Subsequent studies in cadavers and surgical patients firmly established that lymphatic vessels drain extravasated interstitial fluid, also known as lymph, into the venous system at the bilateral lymphovenous junctions. Recent advances revealed that lymphovenous valves and platelet-mediated hemostasis at the lymphovenous junctions maintain life-long separation of the blood and lymphatic vascular systems. Here, we review murine models that exhibit failure of blood–lymph separation to highlight the novel mechanisms and molecular targets for the modulation of lymphatic disorders. Specifically, we focus on the transcription factors, cofactors, and signaling pathways that regulate lymphovenous valve development and platelet-mediated lymphovenous hemostasis, which cooperate to maintain blood–lymph separation.


Similar content being viewed by others
References
Risau W, Flamme I (1995) Vasculogenesis. Annu Rev Cell Dev Biol 11:73–91. https://doi.org/10.1146/annurev.cb.11.110195.000445
Drake CJ, Fleming PA (2000) Vasculogenesis in the day 6.5 to 9.5 mouse embryo. Blood 95:1671–1679
Potente M, Gerhardt H, Carmeliet P (2011) Basic and therapeutic aspects of angiogenesis. Cell 146:873–887. https://doi.org/10.1016/j.cell.2011.08.039
Risau W (1997) Mechanisms of angiogenesis. Nature 386:671–674. https://doi.org/10.1038/386671a0
Bautch VL, Caron KM (2015) Blood and lymphatic vessel formation. Cold Spring Harb Perspect Biol 7:a008268. https://doi.org/10.1101/cshperspect.a008268
Adams RH, Alitalo K (2007) Molecular regulation of angiogenesis and lymphangiogenesis. Nat Rev Mol Cell Biol 8:464–478. https://doi.org/10.1038/nrm2183
Simons M, Eichmann A (2013) Lymphatics are in my veins. Science 341:622–624. https://doi.org/10.1126/science.1243452
Tammela T, Alitalo K (2010) Lymphangiogenesis: molecular mechanisms and future promise. Cell 140:460–476. https://doi.org/10.1016/j.cell.2010.01.045
Loukas M, Bellary SS, Kuklinski M et al (2011) The lymphatic system: a historical perspective. Clin Anat 24:807–816. https://doi.org/10.1002/ca.21194
Sabin FR (1909) The lymphatic system in human embryos, with a consideration of the morphology of the system as a whole. Am J Anat 9:43–91. https://doi.org/10.1002/aja.1000090104
Huntington GS, McClure CFW (1910) The anatomy and development of the jugular lymph sacs in the domestic cat (Felis domestica). Am J Anat 10:177–312. https://doi.org/10.1002/aja.1000100108
Srinivasan RS, Dillard ME, Lagutin OV et al (2007) Lineage tracing demonstrates the venous origin of the mammalian lymphatic vasculature. Genes Dev 21:2422–2432. https://doi.org/10.1101/gad.1588407
Klotz L, Norman S, Vieira JM et al (2015) Cardiac lymphatics are heterogeneous in origin and respond to injury. Nature 522:62–67. https://doi.org/10.1038/nature14483
Stanczuk L, Martinez-Corral I, Ulvmar MH et al (2015) cKit lineage hemogenic endothelium-derived cells contribute to mesenteric lymphatic vessels. Cell Rep 10:1708–1721. https://doi.org/10.1016/j.celrep.2015.02.026
Martinez-Corral I, Ulvmar MH, Stanczuk L et al (2015) Nonvenous origin of dermal lymphatic vasculature. Circ Res 116:1649–1654. https://doi.org/10.1161/CIRCRESAHA.116.306170
Petrova TV, Koh GY (2018) Organ-specific lymphatic vasculature: from development to pathophysiology. J Exp Med 215:35–49. https://doi.org/10.1084/jem.20171868
Ulvmar MH, Makinen T (2016) Heterogeneity in the lymphatic vascular system and its origin. Cardiovasc Res 111:310–321. https://doi.org/10.1093/cvr/cvw175
Uebelhoer M, Boon LM, Vikkula M (2012) Vascular anomalies: from genetics toward models for therapeutic trials. Cold Spring Harb Perspect Med 2:a009688–a009688. https://doi.org/10.1101/cshperspect.a009688
Wassef M, Blei F, Adams D et al (2015) Vascular anomalies classification: recommendations from the international society for the study of vascular anomalies. Pediatrics 136(1):e203–e214. https://doi.org/10.1542/peds.2014-3673
Swartz MA (2001) The physiology of the lymphatic system. Adv Drug Deliv Rev 50:3–20. https://doi.org/10.1016/S0169-409X(01)00150-8
Bernier-Latmani J (2017) Petrova TV (2017) Intestinal lymphatic vasculature: structure, mechanisms and functions. Nat Rev Gastroenterol Hepatol 14(9):510–526. https://doi.org/10.1038/nrgastro.2017.79
Smith ME, Riffat F, Jani P (2013) The surgical anatomy and clinical relevance of the neglected right lymphatic duct: review. J Laryngol Otol 127:128–133. https://doi.org/10.1017/S0022215112002939
Ratnayake CBB, Escott ABJ, Phillips ARJ, Windsor JA (2018) The anatomy and physiology of the terminal thoracic duct and ostial valve in health and disease: potential implications for intervention. J Anat 233:1–14. https://doi.org/10.1111/joa.12811
Ushiwata I, Ushiki T (1990) Cytoarchitecture of the smooth muscles and pericytes of rat cerebral blood vessels. A scanning electron microscopic study. J Neurosurg 73:82–90. https://doi.org/10.3171/jns.1990.73.1.0082
Kinnaert P (1973) Anatomical variations of the cervical portion of the thoracic duct in man. J Anat 115:45–52
Langford RJ, Daudia AT, Malins TJ (1999) A morphological study of the thoracic duct at the jugulo-subclavian junction. J Craniomaxillofac Surg 27:100–104. https://doi.org/10.1016/S1010-5182(99)80021-3
Yalakurthi S, Vishnumukkala TR, Siri CC et al (2013) Anatomical variations of the termination of the thoracic duct in humans. Int J Med Health Sci 2:230–234
Davis HK (1915) A statistical study of the thoracic duct in man. Am J Anat 17:211–244. https://doi.org/10.1002/aja.1000170203
Shimada K, Sato I (1997) Morphological and histological analysis of the thoracic duct at the jugulo-subclavian junction in Japanese cadavers. Clin Anat 10:163–172. https://doi.org/10.1002/(sici)1098-2353(1997)10:3%3c163:aid-ca2%3e3.0.co;2-v
Seeger M, Bewig B, Günther R et al (2009) Terminal part of thoracic duct: high-resolution US imaging. Radiology 252:897–904. https://doi.org/10.1148/radiol.2531082036
Calnan JS, Pflug JJ, Reis ND, Taylor LM (1970) Lymphatic pressures and the flow of lymph. Br J Plast Surg 23:305–317
Pflug J, Calnan J (1968) The valves of the thoracic duct at the angulus venosus. Br J Surg 55:911–916. https://doi.org/10.1002/bjs.1800551208
Parasher VK, Meroni E, Spinelli P (1995) Anatomy of the thoracic duct: an endosonographic study. Gastrointest Endosc 42:188–189. https://doi.org/10.1016/S0016-5107(95)70085-4
Srinivasan RS, Oliver G (2011) Prox1 dosage controls the number of lymphatic endothelial cell progenitors and the formation of the lymphovenous valves. Genes Dev 25:2187–2197. https://doi.org/10.1101/gad.16974811
Geng X, Cha B, Mahamud MR et al (2016) Multiple mouse models of primary lymphedema exhibit distinct defects in lymphovenous valve development. Dev Biol 409:218–233. https://doi.org/10.1016/j.ydbio.2015.10.022
Yang Y, Oliver G (2014) Development of the mammalian lymphatic vasculature. J Clin Investig 124:888–897. https://doi.org/10.1172/JCI71609
Bowles J, Secker G, Nguyen C et al (2014) Control of retinoid levels by CYP26B1 is important for lymphatic vascular development in the mouse embryo. Dev Biol 386:25–33. https://doi.org/10.1016/j.ydbio.2013.12.008
Cha B, Geng X, Mahamud MR et al (2016) Mechanotransduction activates canonical Wnt/β-catenin signaling to promote lymphatic vascular patterning and the development of lymphatic and lymphovenous valves. Genes Dev 30:1454–1469. https://doi.org/10.1101/gad.282400.116
Turner CJ, Badu-Nkansah K, Crowley D et al (2014) Integrin-α5β1 is not required for mural cell functions during development of blood vessels but is required for lymphatic–blood vessel separation and lymphovenous valve formation. Dev Biol 392:381–392. https://doi.org/10.1016/j.ydbio.2014.05.006
Janardhan HP, Milstone ZJ, Shin M et al (2017) Hdac3 regulates lymphovenous and lymphatic valve formation. J Clin Investig 127:4193–4206. https://doi.org/10.1172/JCI92852
Kazenwadel J, Betterman KL, Chong C-E et al (2015) GATA2 is required for lymphatic vessel valve development and maintenance. J Clin Investig 125:2979–2994. https://doi.org/10.1172/JCI78888
Martin-Almedina S, Martinez-Corral I, Holdhus R et al (2016) EPHB4 kinase-inactivating mutations cause autosomal dominant lymphatic-related hydrops fetalis. J Clin Investig 126:3080–3088. https://doi.org/10.1172/JCI85794
Fang J, Dagenais SL, Erickson RP et al (2000) Mutations in FOXC2 (MFH-1), a forkhead family transcription factor, are responsible for the hereditary lymphedema–distichiasis syndrome. Am J Hum Genet 67:1382–1388. https://doi.org/10.1086/316915
Petrova TV, Karpanen T, Norrmén C et al (2004) Defective valves and abnormal mural cell recruitment underlie lymphatic vascular failure in lymphedema distichiasis. Nat Med 10:974–981. https://doi.org/10.1038/nm1094
Sabine A, Agalarov Y, Maby-El Hajjami H et al (2012) Mechanotransduction, PROX1, and FOXC2 cooperate to control connexin37 and calcineurin during lymphatic-valve formation. Dev Cell 22:430–445. https://doi.org/10.1016/j.devcel.2011.12.020
Kanady JD, Munger SJ, Witte MH, Simon AM (2015) Combining Foxc2 and Connexin37 deletions in mice leads to severe defects in lymphatic vascular growth and remodeling. Dev Biol 405:33–46. https://doi.org/10.1016/j.ydbio.2015.06.004
Kanady JD, Dellinger MT, Munger SJ et al (2011) Connexin37 and Connexin43 deficiencies in mice disrupt lymphatic valve development and result in lymphatic disorders including lymphedema and chylothorax. Dev Biol 354:253–266. https://doi.org/10.1016/j.ydbio.2011.04.004
Meens MJ, Sabine A, Petrova TV, Kwak BR (2014) Connexins in lymphatic vessel physiology and disease. FEBS Lett 588:1271–1277. https://doi.org/10.1016/j.febslet.2014.01.011
Karpinich NO, Caron KM (2015) Gap junction coupling is required for tumor cell migration through lymphatic endothelium. Arterioscler Thromb Vasc Biol 35:1147–1155. https://doi.org/10.1161/ATVBAHA.114.304752
Kanady JD, Simon AM (2011) Lymphatic communication: connexin junction, what’s your function? Lymphology 44:95–102
Huang GY, Cooper ES, Waldo K et al (1998) Gap junction-mediated cell–cell communication modulates mouse neural crest migration. J Cell Biol 143:1725–1734. https://doi.org/10.1083/jcb.143.6.1725
Ostergaard P, Simpson MA, Connell FC et al (2011) Mutations in GATA2 cause primary lymphedema associated with a predisposition to acute myeloid leukemia (Emberger syndrome). Nat Genet 43:929–931. https://doi.org/10.1038/ng.923
Kazenwadel J, Secker GA, Liu YJ et al (2012) Loss-of-function germline GATA2 mutations in patients with MDS/AML or MonoMAC syndrome and primary lymphedema reveal a key role for GATA2 in the lymphatic vasculature. Blood 119:1283–1291. https://doi.org/10.1182/blood-2011-08-374363
Spinner MA, Sanchez LA, Hsu AP et al (2014) GATA2 deficiency: a protean disorder of hematopoiesis, lymphatics, and immunity. Blood 123:809–821. https://doi.org/10.1182/blood-2013-07-515528
Hsu AP, Johnson KD, Falcone EL et al (2013) GATA2 haploinsufficiency caused by mutations in a conserved intronic element leads to MonoMAC syndrome. Blood 121:3830–3837. https://doi.org/10.1182/blood-2012-08-452763
Ganapathi KA, Townsley DM, Hsu AP et al (2015) GATA2 deficiency-associated bone marrow disorder differs from idiopathic aplastic anemia. Blood 125:56–70. https://doi.org/10.1182/blood-2014-06-580340
Johnson KD, Hsu AP, Ryu M-J et al (2012) Cis-element mutated in GATA2-dependent immunodeficiency governs hematopoiesis and vascular integrity. J Clin Investig 122:3692–3704. https://doi.org/10.1172/JCI61623
Wozniak RJ, Boyer ME, Grass JA et al (2007) Context-dependent GATA factor function. J Biol Chem 282:14665–14674. https://doi.org/10.1074/jbc.M700792200
Lim K-C, Hosoya T, Brandt W et al (2012) Conditional Gata2 inactivation results in HSC loss and lymphatic mispatterning. J Clin Investig 122:3705–3717. https://doi.org/10.1172/JCI61619
Khandekar M, Brandt W, Zhou Y et al (2007) A Gata2 intronic enhancer confers its pan-endothelia-specific regulation. Development 134:1703–1712. https://doi.org/10.1242/dev.001297
Taniguchi K, Kohno R-I, Ayada T et al (2007) Spreds are essential for embryonic lymphangiogenesis by regulating vascular endothelial growth factor receptor 3 signaling. Mol Cell Biol 27:4541–4550. https://doi.org/10.1128/MCB.01600-06
Deng Y, Atri D, Eichmann A, Simons M (2013) Endothelial ERK signaling controls lymphatic fate specification. J Clin Investig 123:1202–1215. https://doi.org/10.1172/JCI63034
Murtomaki A, Uh MK, Choi YK et al (2013) Notch1 functions as a negative regulator of lymphatic endothelial cell differentiation in the venous endothelium. Development 140:2365–2376. https://doi.org/10.1242/dev.083865
Murtomaki A, Uh MK, Kitajewski C et al (2014) Notch signaling functions in lymphatic valve formation. Development 141:2446–2451. https://doi.org/10.1242/dev.101188
Outeda P, Huso DL, Fisher SA et al (2014) Polycystin signaling is required for directed endothelial cell migration and lymphatic development. Cell Rep 7:634–644. https://doi.org/10.1016/j.celrep.2014.03.064
Cha B, Geng X, Mahamud MR et al (2018) Complementary Wnt sources regulate lymphatic vascular development via PROX1-dependent Wnt/β-catenin signaling. Cell Rep 25:571–584.e5. https://doi.org/10.1016/j.celrep.2018.09.049
Loirand G, Sauzeau V, Pacaud P (2013) Small G proteins in the cardiovascular system: physiological and pathological aspects. Physiol Rev 93:1659–1720. https://doi.org/10.1152/physrev.00021.2012
Garrett TA, van Buul JD, Burridge K (2007) VEGF-induced Rac1 activation in endothelial cells is regulated by the guanine nucleotide exchange factor Vav2. Exp Cell Res 313:3285–3297
Zeng H, Zhao D, Mukhopadhyay D (2002) KDR stimulates endothelial cell migration through heterotrimeric G protein Gq/11-mediated activation of a small GTPase RhoA. J Biol Chem 277:46791–46798. https://doi.org/10.1074/jbc.M206133200
D’Amico G, Jones DT, Nye E et al (2009) Regulation of lymphatic–blood vessel separation by endothelial Rac1. Development 136:4043–4053. https://doi.org/10.1242/dev.035014
Liu X, Gu X, Ma W et al (2018) Rasip1 controls lymphatic vessel lumen maintenance by regulating endothelial cell junctions. Development 145:dev165092. https://doi.org/10.1242/dev.165092
Xu W, Wittchen ES, Hoopes SL et al (2018) Small GTPase Rap1A/B is required for lymphatic development and adrenomedullin-induced stabilization of lymphatic endothelial junctions. Arterioscler Thromb Vasc Biol. https://doi.org/10.1161/atvbaha.118.311645;pagegroup:string:publication
Kimberling WJ, Fain PR, Kenyon JB et al (1988) Linkage heterogeneity of autosomal dominant polycystic kidney disease. N Engl J Med 319:913–918. https://doi.org/10.1056/NEJM198810063191405
Romeo G, Costa G, Catizone L et al (1988) A second genetic locus for autosomal dominant polycystic kidney disease. Lancet 332:8–11. https://doi.org/10.1016/S0140-6736(88)92943-1
Coxam B, Sabine A, Bower NI et al (2014) Pkd1 regulates lymphatic vascular morphogenesis during development. Cell Rep 7:623–633
Bellini C, Donarini G, Paladini D et al (2015) Etiology of non-immune hydrops fetalis: an update. Am J Med Genet 167:1082–1088. https://doi.org/10.1002/ajmg.a.36988
Mackie DI, Mutairi Al F, Davis RB et al (2018) hCALCRL mutation causes autosomal recessive nonimmune hydrops fetalis with lymphatic dysplasia. J Exp Med 215:2339–2353. https://doi.org/10.1084/jem.20180528
Alders M, Al-Gazali L, Cordeiro I et al (2014) Hennekam syndrome can be caused by FAT4 mutations and be allelic to Van Maldergem syndrome—PubMed-NCBI. Hum Genet 133:1161–1167. https://doi.org/10.1007/s00439-014-1456-y
Alders M, Hogan BM, Gjini E et al (2009) Mutations in CCBE1 cause generalized lymph vessel dysplasia in humans. Nat Genet 41:1272–1274. https://doi.org/10.1038/ng.484
Fotiou E, Martin-Almedina S, Simpson MA et al (2015) Novel mutations in PIEZO1 cause an autosomal recessive generalized lymphatic dysplasia with non-immune hydrops fetalis. Nat Commun 6:8085. https://doi.org/10.1038/ncomms9085
Shah S, Conlin LK, Gomez L et al (2013) CCBE1 mutation in two siblings, one manifesting lymphedema-cholestasis syndrome, and the other, fetal hydrops. PLoS One 8:e75770. https://doi.org/10.1371/journal.pone.0075770
Avraamides CJ, Garmy-Susini B, Varner JA (2008) Integrins in angiogenesis and lymphangiogenesis. Nat Rev Cancer 8:604–617. https://doi.org/10.1038/nrc2353
Chen J, Alexander JS, Orr AW (2012) Integrins and their extracellular matrix ligands in lymphangiogenesis and lymph node metastasis. Int J Cell Biol 2012:1–12. https://doi.org/10.1155/2012/853703
Hess PR, Rawnsley DR, Jakus Z et al (2014) Platelets mediate lymphovenous hemostasis to maintain blood–lymphatic separation throughout life. J Clin Investig 124:273–284. https://doi.org/10.1172/JCI70422
Vigl B, Zgraggen C, Rehman N et al (2009) Coxsackie- and adenovirus receptor (CAR) is expressed in lymphatic vessels in human skin and affects lymphatic endothelial cell function in vitro. Exp Cell Res 315:336–347. https://doi.org/10.1016/j.yexcr.2008.10.020
Mirza M, Pang M-F, Zaini MA et al (2012) Essential role of the coxsackie—and adenovirus receptor (CAR) in development of the lymphatic system in mice. PLoS One 7:e37523. https://doi.org/10.1371/journal.pone.0037523
Abtahian F, Guerriero A, Sebzda E et al (2003) Regulation of blood and lymphatic vascular separation by signaling proteins SLP-76 and Syk. Science 299:247–251. https://doi.org/10.1126/science.1079477
Bertozzi CC, Schmaier AA, Mericko P et al (2010) Platelets regulate lymphatic vascular development through CLEC-2–SLP-76 signaling. Blood 116:661–670. https://doi.org/10.1182/blood-2010-02-270876
Sebzda E, Hibbard C, Sweeney S et al (2006) Syk and Slp-76 Mutant mice reveal a cell-autonomous hematopoietic cell contribution to vascular development. Dev Cell 11:349–361. https://doi.org/10.1016/j.devcel.2006.07.007
Suzuki-Inoue K, Kato Y, Inoue O et al (2007) Involvement of the snake toxin receptor CLEC-2, in podoplanin-mediated platelet activation, by cancer cells. J Biol Chem 282:25993–26001. https://doi.org/10.1074/jbc.M702327200
Suzuki-Inoue K, Fuller GLJ, García A et al (2006) A novel Syk-dependent mechanism of platelet activation by the C-type lectin receptor CLEC-2. Blood 107:542–549. https://doi.org/10.1182/blood-2005-05-1994
Finney BA, Schweighoffer E, Navarro-Nuñez L et al (2012) CLEC-2 and Syk in the megakaryocytic/platelet lineage are essential for development. Blood 119:1747–1756. https://doi.org/10.1182/blood-2011-09-380709
Suzuki-Inoue K, Inoue O, Ding G et al (2010) Essential in vivo roles of the C-type lectin receptor CLEC-2: embryonic/neonatal lethality of CLEC-2-deficient mice by blood/lymphatic misconnections and impaired thrombus formation of CLEC-2-deficient platelets. J Biol Chem 285:24494–24507. https://doi.org/10.1074/jbc.M110.130575
Herzog BH, Fu J, Wilson SJ et al (2013) Podoplanin maintains high endothelial venule integrity by interacting with platelet CLEC-2. Nature 502:105–109
Uhrin P, Zaujec J, Breuss JM et al (2010) Novel function for blood platelets and podoplanin in developmental separation of blood and lymphatic circulation. Blood 115:3997–4005. https://doi.org/10.1182/blood-2009-04-216069
Ichise H, Ichise T, Ohtani O, Yoshida N (2009) Phospholipase Cgamma2 is necessary for separation of blood and lymphatic vasculature in mice. Development 136:191–195. https://doi.org/10.1242/dev.025353
Kato Y, Kaneko MK, Kunita A et al (2008) Molecular analysis of the pathophysiological binding of the platelet aggregation-inducing factor podoplanin to the C-type lectin-like receptor CLEC-2. Cancer Sci 99:54–61. https://doi.org/10.1111/j.1349-7006.2007.00634.x
May F, Hagedorn I, Pleines I et al (2009) CLEC-2 is an essential platelet-activating receptor in hemostasis and thrombosis. Blood 114:3464–3472. https://doi.org/10.1182/blood-2009-05-222273
Fuller GLJ, Williams JAE, Tomlinson MG et al (2007) The C-type lectin receptors CLEC-2 and Dectin-1, but not DC-SIGN, signal via a novel YXXL-dependent signaling cascade. J Biol Chem 282:12397–12409. https://doi.org/10.1074/jbc.M609558200
Spalton JC, Mori J, Pollitt AY et al (2009) The novel Syk inhibitor R406 reveals mechanistic differences in the initiation of GPVI and CLEC-2 signaling in platelets. J Thromb Haemost 7:1192–1199. https://doi.org/10.1111/j.1538-7836.2009.03451.x
Séverin S, Pollitt AY, Navarro-Nuñez L et al (2011) Syk-dependent phosphorylation of CLEC-2 a novel mechanism of hem-immunoreceptor tyrosine-based activation motif signaling. J Biol Chem 286:4107–4116. https://doi.org/10.1074/jbc.M110.167502
Carramolino L, Fuentes J, García-Andrés C et al (2010) Platelets play an essential role in separating the blood and lymphatic vasculatures during embryonic angiogenesis. Circ Res 106:1197–1201
Manne BK, Badolia R, Dangelmaier C et al (2015) Distinct pathways regulate Syk protein activation downstream of immune tyrosine activation motif (ITAM) and hemITAM receptors in platelets. J Biol Chem 290:11557–11568. https://doi.org/10.1074/jbc.M114.629527
Zhang Y, Daubel N, Stritt S, Makinen T (2018) Transient loss of venous integrity during developmental vascular remodeling leads to red blood cell extravasation and clearance by lymphatic vessels. Development 145:dev156745. https://doi.org/10.1242/dev.156745
Fu J, Gerhardt H, McDaniel JM et al (2008) Endothelial cell O-glycan deficiency causes blood/lymphatic misconnections and consequent fatty liver disease in mice. J Clin Investig 118:3725–3737. https://doi.org/10.1172/JCI36077
Bianchi R, Russo E, Bachmann SB et al (2017) Postnatal deletion of podoplanin in lymphatic endothelium results in blood filling of the lymphatic system and impairs dendritic cell migration to lymph nodes. Arterioscler Thromb Vasc Biol 37:108–117. https://doi.org/10.1161/ATVBAHA.116.308020
Crosswhite PL, Podsiadlowska JJ, Curtis CD et al (2016) CHD4-regulated plasmin activation impacts lymphovenous hemostasis and hepatic vascular integrity. J Clin Investig 126:2254–2266. https://doi.org/10.1172/JCI84652
Welsh JD, Kahn ML, Sweet DT (2016) Lymphovenous hemostasis and the role of platelets in regulating lymphatic flow and lymphatic vessel maturation. Blood 128:1169–1173. https://doi.org/10.1182/blood-2016-04-636415
Chen C-Y, Bertozzi C, Zou Z et al (2012) Blood flow reprograms lymphatic vessels to blood vessels. J Clin Investig 122:2006–2017. https://doi.org/10.1172/JCI57513
Kiefer F, Brumell J, Al-Alawi N et al (1998) The Syk protein tyrosine kinase is essential for Fcγ receptor signaling in macrophages and neutrophils. Mol Cell Biol 18:4209–4220. https://doi.org/10.1128/MCB.18.7.4209
Turner M, Mee PJ, Costello PS et al (1995) Perinatal lethality and blocked B-cell development in mice lacking the tyrosine kinase Syk. Nature 378:298–302. https://doi.org/10.1038/378298a0
Cheng AM, Rowley B, Pao W et al (1995) Syk tyrosine kinase required for mouse viability and B-cell development. Nature 378:303–306. https://doi.org/10.1038/378303a0
Sweet DT, Jiménez JM, Chang J et al (2015) Lymph flow regulates collecting lymphatic vessel maturation in vivo. J Clin Investig 125:2995–3007. https://doi.org/10.1172/JCI79386
Bäckhed F, Crawford PA, O’Donnell D, Gordon JI (2007) Postnatal lymphatic partitioning from the blood vasculature in the small intestine requires fasting-induced adipose factor. Proc Natl Acad Sci USA 104:606–611. https://doi.org/10.1073/pnas.0605957104
Acknowledgements
We gratefully acknowledge Zachary J. Milstone for critical reading of the article. C.M.T is supported by National Heart, Lung, and Blood Institute grants R01 HL141377 (to C.M.T). We apologize to our colleagues whose work could not be discussed due to space limitations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Janardhan, H.P., Trivedi, C.M. Establishment and maintenance of blood–lymph separation. Cell. Mol. Life Sci. 76, 1865–1876 (2019). https://doi.org/10.1007/s00018-019-03042-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-019-03042-3