Abstract
Objective and design
Our research aimed to investigate the role of CD14 in pulmonary infection by Achromobacter xylosoxidans in an experimental murine model.
Methods
C57Bl/6 or CD14-deficient mice were infected intratracheally with non-lethal inoculum of A. xylosoxidans. At times 1, 3 and 7 days after infection, lungs, bronchoalveolar lavage and blood were collected. CD14 gene expression was determined by RT-PCR. The bacterial load in the lungs was assessed by counting colony forming units (CFU). Cytokines, chemokines, lipocalin-2 and sCD14 were quantified by the ELISA method. Inflammatory infiltrate was observed on histological sections stained with HE, and leukocyte subtypes were assessed by flow cytometry. In another set of experiments, C57Bl/6 or CD14-deficient mice were inoculated with lethal inoculum and the survival rate determined.
Results
CD14-deficient mice are protected from A. xylosoxidans-induced death, which is unrelated to bacterial load. The lungs of CD14-deficient mice presented a smaller area of tissue damage, less neutrophil and macrophage infiltration, less pulmonary edema, and a lower concentration of IL-6, TNF-α, CXCL1, CCL2 and CCL3 when compared with lungs of C57Bl/6 mice. We also observed that A. xylosoxidans infection increases the number of leukocytes expressing mCD14 and the levels of sCD14 in BALF and serum of C57Bl/6-infected mice.
Conclusions
In summary, our data show that in A. xylosoxidans infection, the activation of CD14 induces intense pulmonary inflammatory response resulting in mice death.
Similar content being viewed by others
Introduction
A. xylosoxidans is a Gram-negative, mobile, biofilm-forming bacillus and resistant to various antibiotics which cause recurrent pulmonary infections in patients with cystic fibrosis (CF), contributing to disease progression [1, 2]. CF patients infected with A. xylosoxidans present high amounts of cytokines in serum and sputum in comparison with health individuals [3]. Furthermore, other authors have shown that in vitro exposure of human lung lineage cells with cytotoxins free of lipopolysaccharide (LPS) extracted from A. xylosoxidans, can induce the production of cytokines, vacuolization and lung cell death [4]. Recently, our group showed that leukotriene B4 (LTB4) has a protective role in a mice model of A. xylosoxidans infection by inducing the production of α-defensin-1, an antimicrobial peptide responsible for reduction of bacterial load in the lungs, and control of inflammation [5]. Together, these data seem to point to the importance of the inflammatory process in the outcome of A. xylosoxidans infection.
The recognition of LPS, the main component of the wall of Gram-negative bacteria, is well described [6, 7]. Soluble Lipopolysaccharide-Binding Protein (LPB) binds to bacterial membrane sites rich in LPS, forming aggregates, which are recognized by CD14 and then presented to the MD2-TLR4 complex, resulting in the activation of transcription factors, such as NF-κB, and induction of pro-inflammatory genes [8, 9]. CD14 is a myeloid differentiating glycoprotein, expressed mainly in immune cells, such as macrophages, monocytes and neutrophils [10, 11], although it is also expressed in non-immune cells, such as epithelial cells [12] and hepatocytes [13]. CD14 can be anchored to the membrane (mCD14) by a tail of glycosylphosphatidylinositol (GPI) or soluble (sCD14) in plasma and biological fluids [14]. In addition to being considered a co-receptor in the recognition of LPS, studies have shown that CD14 is important in the clearance of apoptotic cells [15], potentiates cardiovascular and metabolic complications in obesity [16] and mediate lung inflammation induced by scorpion venom as previously reported by our group [17, 18].
CD14 signaling has divergent impacts, depending on stimulus and tissue location [19]. Previously, we showed that CD14 controls macrophage metabolism, which varies according to the stimulus and origin of these cells [20]. In addition, the blockade or deficiency of CD14 has been shown to confer resistance to mortality induced by systemic infection of E. coli and endotoxemic shock induced by LPS, with reduction in bacteremia and levels of TNF-α and IL-6 in serum [21,22,23]. In contrast, the role of CD14 in the outcome of lung infections caused by Gram-negative bacteria still controversial [24]. Despite advances in understanding some aspects of A. xylosoxidans infection in recent years, the mechanisms involved in the recognition of this bacillus and the receptors involved, remain poorly understood. Therefore, in this work, we evaluated the role of CD14 in a mice model of pneumonia induced by A. xylosoxidans.
Materials and methods
Mice
C57Bl/6 (wild-type) and Cd14−/− mice aged 8–9 weeks and weighing 24–26 g were purchased from Jackson Laboratory (Bar Harbor, ME, USA) and housed in ventilated shelf with free access to water and food at the Faculty of Pharmaceutical Sciences of Ribeirão Preto, University of São Paulo (FCFRP-USP). All procedures performed were approved by the FCFRP Animal Use Ethics Committee (CEUA) under protocol number 17.1.820.60.0.
A. xylosoxidans culture
The LMG1836 strain of A. xylosoxidans from the Belgian Co-ordinated Collections of Micro-organisms BCCM/LMG was used. For each experiment, the strain was grown in brain and heart infusion broth (BHI) with agar (Difco, Detroit, MI, USA) and maintained at 37 ºC for 18 h. The colonies were resuspended in sterile PBS and the number of bacteria was quantified by spectrophotometer (600 nm) for later infection [5].
Intratracheal infection, collection of bronchoalveolar lavage fluid (BALF), blood collection and experimental design
C57Bl/6 and Cd14−/− mice were anesthetized via intraperitoneal (i.p.) administration of ketamine (75 mg/kg body weight) and xylazine (10 mg/kg) and infected intratracheally (i.t.) with 100 µL of bacterial inoculum containing 2.0 × 107 bacilli (non-lethal inoculum) in the kinetic experiments, for assessment of lung pathology, cell recruitment and production of inflammatory mediators in lungs and blood. On days 1, 3 and 7 d.p.i., the mice were anesthetized and euthanized by cervical dislocation to collect BALF (n = 3–7 mice/group). In another set of experiments (n = 3–6 mice/group), blood and lungs were collected without performed the BALF. The control groups received i.t. 100 µL of sterile PBS. The blood was collected in a tube without anticoagulant and centrifuged at 1500g for 12 min, at 4 ºC, to obtain the serum. To determine the survival curve, a separate group of C57Bl/6 and Cd14−/− mice (n = 8/group) were infected with 6.3 × 107 bacilli and the mortality monitored daily.
Histopathological analysis of the lungs and immunohistochemistry
The middle right lobe of the lungs of the mice from the different groups were removed and fixed in 10% buffered formaldehyde for 7 days and then prepared in paraffin blocks. Histological sections of 5 µM thick were stained with hematoxylin and eosin (HE). Seven random photos were taken of each lung (400 × magnification) to assess the area of tissue injury using ImageJ software (U.S. NIH, Bethesda, MD, USA) as described [25]. Immunohistochemistry was performed to mark CD14 in the lungs of C57Bl/6 mice. The sections were dewaxed and incubated with peroxidase blocking reagent. The sections were treated with 1% bovine serum albumin (BSA) to block nonspecific reactions. Clone [1H5D8] anti-CD14 antibody (Abcam, Burlingame, CA, USA) was applied to the cuts followed by improved horseradish peroxidase (HRP) based on improved luminol (ECL) (GE Healthcare, Chicago, IL, USA). The reaction was developed with diaminobenzidine (DAB) (Vector Laboratories, Burlingame, CA, USA) and the sections were counterstained with HE.
Bacterial burden and flow cytometry of lungs cells
The left upper pulmonary lobe was digested at 37ºC for 45 min in 1 mL per lung of digestion buffer [RPMI 1640, 0.05 mg/mL liberase (Roche, Basel, Switzerland) and DNAse 0.5 mg/mL (Sigma–Aldrich, St. Louis, Missouri, USA)]. 50 µL of these suspensions were diluted and cultivated on BHI agar and maintained at 37 ºC for 36 h to count the CFU. The bacterial burden was expressed as an absolute number of CFU/gram of lung. The rest of the suspensions were filtered through a cell filter with 100 µm pore (BD Biosciences, Franklin Lakes, New Jersey, USA) to characterize the lung cells. The resulting suspension was centrifuged at 300g at 4 ºC for 10 min. The red cells present were lysed with ammonium potassium chloride (ACK). The number of viable cells was determined to 2 × 106 using Trypan blue and Neubauer chamber [26]. Following fixation and blocking, the antibodies used were: CD11b (clone: M1/70), CD11c (clone: N418), F4/80 (clone: BM8), MHC-II (clone: M5/114.15.2), CD14 (clone: rmC5-3), Ly6G (clone: 1A8), CD45 (clone: 30F11), CX3CR1 (clone: SA011F11), Ly6C (clone: HK1.4), all purchased from eBioscience (San Diego, CA) or BD Biosciences (Franklin Lakes, New Jersey, USA). After labeling, the cells were resuspended in Cytofix fixation buffer (BD Biosciences Franklin Lakes, New Jersey, USA). 2 × 106 events were acquired on the LSR Fortessa cytometer (BD Biosciences, Franklin Lakes, New Jersey, USA) and analyzed using FlowJo software v.10.0.7 (BD Biosciences, Franklin Lakes, New Jersey, USA).
Quantification of sCD14
The BALF was centrifuged at 500 g for 10 min at 4ºC and the supernatant was frozen at – 80 ºC. To quantify sCD14 in the BALF supernatant and animal serum, the CD14 quantikine ELISA kit mouse (range 62.5–4000 pg/mL; R&D Systems, Minnesota, MN, USA) was used and the optical density was read at 450 nm in a spectrophotometer, according to the manufacturer's specifications.
Quantification of cytokine and total proteins
The upper and lower right lung lobes were homogenized in 2 mL RPMI-I with Ultra-Turrax (IKA, Labortechnik, Staufen, Germany) and the suspensions obtained were centrifuged. The supernatants of the lung homogenates and the serum were used for quantification of cytokines (IL-6, TNF-α, IL-1α, IL-1β, IL-17, IFN-γ) and chemokines (CXCL1, CCL2, CCL3) by ELISA (R&D Systems, Minnesota, MN, USA), according to the manufacturer's instructions. Total proteins were quantified in the lungs and BALF supernatants, using the Bradford colorimetric method (Coomassie reagent, Pierce Chemical, Rockford, IL, USA), according to the manufacturer's instructions.
Nitrite quantification
For indirect quantification of nitric oxide, the supernatants of the BALF and lung homogenates were used to quantify nitrite (NO2−) using the Griess method as described [27].
RNA extraction from the lungs and qRT-PCR
To evaluate the CD14 gene expression in C57Bl/6 mice, the lower left lobe of the lungs was removed and homogenized for mRNA extraction with Purelink RNA MiniKit kit (Life Technologies, Carlsbad, California, USA) according to the manufacturer's recommendations. The cDNA was synthesized using the High Capacity cDNA Reverse Transcription kit (Applied Biosystems, Waltham, MA, USA). Real-time quantitative PCR was performed using the TaqMan system in Step One Plus (Applied Biosystems, Waltham, MA, USA). The Cd14 expression values (primer: Mm00438094_g1; Life Technologies—CA, EUA) were normalized by the expression values of the constitutive Gapdh gene (primer: Mm99999915_g1; Life Technologies—CA, EUA). For representation of the results, the gene expression of the uninfected mice was considered as reference samples, with 2−ΔΔCT equal to 1 [28].
Statistical analysis
Statistical analysis was performed using the GraphPad Prism software (Gran Pad Software Inc., San Diego, CA, USA) by ANOVA one-way with multiple Tukey’s comparisons. For analysis of the survival curves, the Log-Rank test and Mantel-Cox test were performed in the post-test. Differences were considered significant when p values < 0.05. The correlation analysis between sCD14 and total proteins was performed using Pearson r statistical test.
Results
The absence of CD14 protects against A. xylosoxidans-induced mortality without changing the bacterial load
To investigate whether A. xylosoxidans infection increases CD14 in the lungs, we infected C57Bl/6 mice intratracheally with 2.0 × 107 A. xylosoxidans bacilli (non-lethal inoculum) and evaluated CD14 expression. As shown in Fig. 1A, the Cd14 gene was up-regulated in the lungs on days 1 and 3 after infection when compared to the uninfected group (PBS control group). Similarly, CD14 protein labeling in the lungs was increased after infection (Fig. 1B). The role of CD14 in pneumonia induced by Gram-negative bacteria is controversial, in some models it is harmful, as it induces intense pulmonary inflammation, in others it is essential, as it induces microbicidal mechanisms and control of bacterial load [24, 29]. Therefore, to assess the role of CD14 in our pneumonia model, we used CD14-deficient mice. To evaluate the survival curve, mice were infected with 6.3 × 107 A. xylosoxidans bacilli (lethal inoculum), and as shown in Fig. 1C, on the 5th day after infection 100% of C57Bl/6 mice died, whereas all mice deficient for CD14 survived 7 days after infection. Surprisingly, we did not detect differences in bacterial load in the lungs (Fig. 1D) and in the production of nitric oxide (data not shown), but we observed reduced production of lipocalin-2 in the lungs of CD14-deficient mice on the 3 d.p.i. when compared to the C57Bl/6 animals (Fig. 1E). Taken together, our data show that A. xylosoxidans infection increases CD14 expression, and that the absence of this molecule protects mice from pneumonia-induced lung injury and mortality.
CD14 is increased in the lungs after infection and mediates A. xylosoxidans-induced mortality, but does not change the bacterial burden. A. Cd14 gene expression in the lungs of C57Bl/6 mice infected with 2.0 × 107 CFU (non-lethal inoculum) evaluated by RT-PCR. The values were normalized by the values of Gapdh expression. B. Representative photomicrographs showing the expression of CD14 in the lungs of C57Bl/6 mice at 1 and 3 d.p.i., stained with anti-CD14 by immunohistochemistry (400 × magnification, scale bar: 50 µm). C. The survival rate of C57Bl/6 and Cd14−/−-infected mice with 6.3 × 107 CFU (lethal inoculum) was monitored during 7 days post-infection. D. Bacterial burden determined by A. xylosoxidans CFU counts in the lungs of C57Bl/6 or Cd14−/− mice infected with 2.0 × 107 bacilli (non-lethal inoculum). E. Concentrations of lipocalin-2 measured by ELISA in lungs of infected mice. A, B, D and E are representative of two independent experiments (n = 4–5 animals), data were analyzed by one-way analysis of variance (ANOVA) with Tukey’s multiple comparisons test, and are expressed as mean ± s.e.m. *p < 0.05. C is representative of three independent experiments (n = 8/experiment) analyzed by Log-rank test and Mantel-Cox post-test. *infected vs PBS, #Cd14.−/− vs C57Bl/6
CD14 deficiency protects mice from lung injury induced by A. xylosoxidans infection.
We observed that CD14-deficient mice presented less lung injury and edema and are protected from mortality, despite showing no difference in bacterial load when compared to C57Bl/6 mice. To investigate a putative mechanism that induces mortality in C57Bl/6 mice, we evaluated the inflammation in the lungs of infected mice. Macroscopically, the lungs of infected C57Bl/6 mice showed hemorrhagic foci and more intense lung damage (Fig. 2A) and more pronounced lung edema (Fig. 2B) when compared to CD14-deficient mice. We confirmed the reduction in lung inflammation in the absence of CD14 through histological analysis. As we reported before [5], we observed that A. xylosoxidans infection induces intense recruitment of leukocytes to the lungs of C57Bl/6 mice, especially at 3 d.p.i.; however, CD14-deficient animals presented significant reduction in cellular recruitment (Fig. 2C), resulting in reduced damage in the architecture of the lung (Fig. 2D). In addition, Cd14−/− mice exhibited lower BALF total protein concentration on the 3 d.p.i. when compared to C57Bl/6 mice, indicating less vascular leakage in the lungs (Fig. 2E).
The absence of CD14 restrains pulmonary inflammation induced by A. xylosoxidans. A. Macroscopic aspect of the lungs of mice infected with 2,0 × 107 A. xylosoxidans at 3 d.p.i. showing the intensity of lung damage. B. Weight of the lungs of mice infected with A. xylosoxidans. C. Representative photomicrographs of the lung pneumonia of mice infected with A. xylosoxidans, stained with HE, at 100× (scale bar:100 µm) and 400× (scale bar: 50 µm, in inset) magnification. D. Percentage of inflamed area in the lungs of mice infected with A. xylosoxidans, analysis performed by ImageJ software. E. Total proteins in BALF of infected mice. A, B, E and F are representative of two independent experiments (n = 4–6), C, D are representative of one experiment (n = 4–6). Data were analyzed by one-way ANOVA with Tukey’s multiple comparisons test, and are expressed as mean ± s.e.m. *p < 0.05.* infected vs PBS, # Cd14.−/− vs C57Bl/6
Absence of CD14 alters the population of cells recruited into the lungs
To evaluate the impact of CD14 deficiency on the population of cells recruited during A. xylosoxidans infection, C57BL/6 and Cd14−/− mice were infected with 2 × 107 CFU and cell subpopulations were characterized in the lungs, applying the flow cytometric gating hierarchy shown in the Suppl. 1A. Initially, we analyze the complexity of lung cells in a two-dimensional way and displayed their distribution in relation to the CD45+ population. The t-SNE map of the populations of some innate cells was produced according to the combination of surface markers expressed by each population (Fig. 3A). The analysis of the frequency of these cells in the lungs of mice infected with A. xylosoxidans showed that CD14-deficiency promotes a reduction in alveolar macrophages accompanied by a significant increase in dendritic cells at 3 d.p.i., and reduction of patrolling monocytes, at 7 d.p.i. (Suppl 2A-D). In addition, although we did not observe differences in the frequency of neutrophils between C57Bl/6 and Cd14−/− mice, CD14-deficiency results in significant decrease in the absolute number of neutrophils in the lungs, at 1 and 3 d.p.i. (Fig. 3B), whereas the number of interstitial (Fig. 3C) and alveolar macrophages (Fig. 3D) only decreased at 3 d.p.i. The number of inflammatory monocytes was significantly reduced in the Cd14−/− mice when compared with C57Bl/6 mice at 1 d.p.i. (Fig. 3D). We did not observe differences in the absolute number of dendritic cells between C57Bl/6 and Cd14−/− mice (Suppl. 2E). Interestingly, the number of patrolling monocytes was reduced at 7 d.p.i. in the lungs of Cd14−/− mice (Suppl. 2F). These data show that CD14 plays an important role for the influx of leukocytes into the lungs after A. xylosoxidans infection.
CD14 modulates the recruitment of neutrophils, macrophages and DCs to the A. xylosoxidans-infected lungs. A. t-SNE map show the representative neutrophils (CD45+ CD11b+ Ly6G+), interstitial macrophages (CD45+ CD11b+ F4/80+MHC-II+), alveolar macrophages (CD45+ F4/80+ CD11c+ Siglec-F+) and DCs (CD45+ CD11c+ CD11b+ MHC-II+). Absolute number of neutrophils B, interstitial macrophages C, alveolar macrophages D and inflammatory monocytes E in lungs. Data are representative of two independent experiments (n = 4–6), analyzed by one-way ANOVA with Tukey’s multiple comparisons test, and are expressed as mean ± s.e.m. *p < 0.05.* infected vs PBS, # Cd14.−/− vs C57Bl/6
CD14 signaling induces chemokines and pro-inflammatory cytokines during A. xylosoxidans infection
The rapid recruitment of leukocytes to the lungs after an infection is coordinated by the production of chemokines by the resident cells [30]. In agreement with the decrease in immune cells in the lungs of CD14-deficient mice, the amount of CXCL1, CCL2 and CCL3 chemokines was also reduced at 3 d.p.i. (Fig. 4A-–C). CD14 signaling regulates the production of cytokines and others mediators of inflammation [31, 32]. The leukocytes recruited during an infection, such as neutrophils, macrophages and DCs, are important sources of pro-inflammatory cytokines, which potentiate the inflammatory response at the site of infection and can also reach the systemic circulation [33]. Based on this, we evaluated the impaction of the absence of CD14 on the production of cytokines in the lungs and the serum after A. xylosoxidans infection. Compared to C57Bl/6 mice, IL-6 was reduced at 3 d.p.i. in the lungs of Cd14−/− mice (Fig. 4A); on the other hand, TNF-α modulation varied with time, at 1 d.p.i. there was less production of this cytokine in the lungs of Cd14−/− mice, but at 3 d.p.i. TNF-α increased in the absence of CD14 (Fig. 4B). Although the infection induced production of IL-1α (Fig. 4C), IL-1β (Fig. 4D), IL-17 (data not shown) and IFN-γ (data not shown) in the lungs of C57Bl/6 mice, we did not observe differences when compared to Cd14−/− animals. In serum, we observed the reduction of IL-6 at 1 d.p.i. in CD14-deficient mice (Fig. 4E), whereas TNF-α was reduced at 3 d.p.i when compared to C57Bl/6 mice (Fig. 4F). Taken together, these data show that CD14 is a strong inducer of pro-inflammatory mediators in response to A. xylosoxidans infection.
The absence of CD14 impacts in the production of inflammatory mediators of mice infected with A. xylosoxidans. Concentration of chemokines CXCL1 A, CCL2 B and CCL3 C, and cytokines in the lungs, IL-6 D, TNF-α E, IL-1α F, IL-1β G, and IL-6 H and TNF-α I in the serum, determined by ELISA. A–G are representative of two independent experiments (n = 4–6), H-I are representative of one experiment (n = 3–5). Data were analyzed by one-way ANOVA with Tukey’s multiple comparisons test, and are expressed as mean ± s.e.m. *p < 0.05.* infected vs PBS, #Cd14.−/− vs C57Bl/6
A. xylosoxidans infection increases CD14+ leukocytes in the lung and sCD14 in BALF and serum
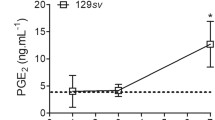
So far, our data show that infection by A. xylosoxidans increases the expression of CD14 in the lung parenchyma and that this receptor is essential to induces inflammation and injury of the lungs. Our next step was to investigate the main source of CD14 during the infection, and for that, we infected C57Bl/6 mice with 2.0 × 107 CFU of A. xylosoxidans and evaluate of CD14 in distinct forms. When we evaluated the absolute number of membrane-bound CD14+ leukocytes (mCD14) recruited to the lung, we observed that the infection induces an increase in neutrophils (Fig. 5A), interstitial (Fig. 5B) and alveolar macrophages (Fig. 5C) expressing CD14 at 3 d.p.i. when compared to the PBS group. On the other hand, we did not observe variations in the median fluorescence intensity in the evaluated macrophages, but only a decrease in neutrophils at 7 d.p.i. when compared to the uninfected group (Suppl. 3). As CD14 is also secreted in the soluble form (sCD14) after an inflammatory stimulus [34], we also evaluated sCD14. Interestingly, in C57Bl/6 BALF infected with A. xylosoxidans there is an increase in sCD14 at all times evaluated, peaking at 3 d.p.i. (Fig. 5D). We also detected increase in sCD14 at 3 d.p.i. in the serum (Fig. 5E), indicating that the intense inflammatory process that occurs in the lungs may reflect on the blood circulation. Interesting, the increase in sCD14 after infection positively correlates with the augment of total proteins in BALF at 3 d.p.i., indicating pulmonary edema (Fig. 5F), and thus, impaired lung function, which leads to mouse mortality.
A. xylosoxidans infection increases mCD14 in leukocytes and sCD14 in lung and serum. Absolute number of neutrophils A, interstitial B and alveolar macrophages C expressing CD14 in lungs evaluated by flow cytometry. sCD14 levels in BALF D and serum E detected by ELISA. F. Correlation study between sCD14 in lung and total proteins in BALF at 3 d.p.i. A–E are representative of two independent experiments (n = 3–7), data were analyzed by one-way ANOVA with Tukey’s multiple comparisons test, and are expressed as mean ± s.e.m. *p < 0.05. *infected vs PBS. F correlation was performed using Pearson r statistical test. Each spot is representative of each mouse (n = 6) and the values of r and p are specified in the graph
Discussion
Recognition of PAMPs by immune cells is the first step to start the immune response, whose objective is to eliminate the pathogen and to restore the homeostasis [35, 36]. Innate immunity receptors, such as TLRs, are sensors that detect molecules expressed by pathogens, such as LPS. This molecule is the main component of the outer membrane of Gram-negative bacteria, and is classically recognized by TLR4 and the CD14 co-receptor [6, 37]. The role of CD14 in the outcome of infections by Gram-negative bacteria is controversial and may be related to the induction of a protective immune response or exacerbation of inflammation [19, 24]. In this study, we characterized for the first time the deleterious role of CD14 in pulmonary infection induced by A. xylosoxidans, an emerging nosocomial bacillus whose host responses are not yet to be elucidated.
Previous studies have shown that in pulmonary diseases induced by infection there is an increase in membrane and soluble CD14 expression [38,39,40]. However, there are conflicting results, reinforcing the fact that CD14 expression and its role varies according to the stimulus and site of infection [19, 24]. Some studies show that CD14 has a protective role in the intestine, by increasing the intestinal barrier function in a colitis model [41], and by controlling the bacterial burden of Shigella flexneri [42]. In contrast, in sepsis models, in LPS-induced endotoxemia or lung infections, CD14 activation appears to have a deleterious role [21, 22, 43, 44], despite a study showing that in cecal ligation and puncture (CLP)-induced sepsis the P2X7 purinergic receptor maintains high levels of CD14 in serum, which contributes to the control of bacterial dissemination [45]. Here, we show that beside A. xylosoxidans inducing a significant increase in the expression of CD14 in the lung parenchyma (at 1 and 3 d.p.i.), its absence attenuates inflammation, as observed by the decreases in leukocyte influx, production of inflammatory mediators, lung damage and lipocalin-2. Lipocalin-2, also known as neutrophil gelatinase-associated lipocalin (NGAL), is a protein normally present in neutrophil granules, but can also be expressed in macrophages, and it is associated with antibacterial activity and intense injury and inflammation [46]. Interesting, CD14 absence did not interfered with the bacterial load, suggesting that CD14 is more related to the induction of the inflammatory process than to bacterial clearance in this model. Similarly, CD14-deficient mice with pneumonia caused by Acinetobacter baumannii also show a reduction in polymorphonuclear cells (PMNs) and TNF-α in the BALF, but, contrary to our findings, there is an increase in the bacterial load in the lungs in the first hours after infection, indicating that CD14 may be relevant only in the first hours to control bacterial burden [47]. Interesting, CD14-deficient neutrophils infected with Burkholderia pseudomallei have the same phagocytic capacity as neutrophils from non-deficient animals, suggesting that the CD14-dependent bacterial load reduction mechanism does not occur via phagocytosis and killing capacity [44], but it is associated with increased release of trappin-2 in the lungs, an essential antimicrobial peptide in the elimination of P. aeruginosa [48].
The influx of neutrophils into the lungs is important for the control of an infection, but if exacerbated, it can contribute to lung damage through the release of NETs and enzymes with proteolytic activity, such as neutrophil elastase [49], or the release of lipocalin-2 and other molecules that increase chemokine production by PMNs [50]. After A. xylosoxidans infection, we observed that CD14-deficient mice show a reduction in lipocalin-2, as well as a lower number of neutrophils in the lungs, in addition to less pulmonary damage, resulting in longer survival rate than wild-type animals. In agreement with our results, the lung parenchyma of CD14-deficient animals is more preserved during S. pneumoniae infection when compared to WT mice, in addition to having a lower concentration of total proteins in the lungs, and a reduction in IL-1β, IL-6 and CXCL1 in lungs and plasma of infected mice [51]. In tuberculosis, CD14 also mediates PMN recruitment and release of pro-inflammatory cytokines in the lungs, culminating in lung injury and higher animal mortality [52].
CD14 was first described as anchored to the membrane of macrophages and monocytes, but after inflammatory stimuli such as LPS, CD14 can be released in soluble form via the action of proteases or even after escaping from binding to GPI in post-translational modifications [29, 53]. Defining a pattern of CD14 expression in leukocytes from pneumonia patients or from infected mice is a challenge. Patients with tuberculosis have lower CD14 expression on monocytes when compared to healthy individuals [54], and similarly, mCD14 expression is reduced in alveolar macrophages from mice infected with E. coli when compared to cells from wild-type mice [55]. In contrast, the expression of mCD14 on monocytes and macrophages of children with pneumonia is higher when compared to the control group [56]. In our model of pulmonary infection by A. xylosoxidans, although we did not observe an increase in CD14 MFI on the surface of the evaluated leukocytes, we found an increase in the absolute number of neutrophils and macrophages expressing CD14 that are recruited to the lung, suggesting that the increase in cells capable of signaling via mCD14 contribute to the exacerbation of pulmonary inflammation. sCD14 is considered a potential marker of pneumonia in children [56] and a predictor of severity of coronavirus disease 2019 (COVID-19) [57]. Furthermore, sCD14 is considered an acute phase marker [34], and it was even shown that this molecule is capable of inducing pro-inflammatory cytokines independent of LPS in CF patients, contributing to the persistence of inflammation in these patients [58, 59]. Corroborating these findings, we observed that A. xylosoxidans induces sCD14 release in the BALF and serum of infected animals, suggesting that part of mCD14 of leukocytes or others cells, such epithelial cells, is shedding to the soluble profile during infection. The dynamics of sCD14 release by other leukocytes and non-immune cells needs to be further investigated.
Taken together, our findings highlight the detrimental role of CD14 in A. xylosoxidans-induced pneumonia, mediated by pulmonary and systemic release of sCD14, which likely maintains leukocyte recruitment to the lungs and impairs pulmonary homeostasis. Furthermore, these results reinforce that CD14 inhibition may be a possible alternative therapy for patients with chronic lung inflammation caused by A. xylosoxidans.
References
Yabuuchi E, Oyama A. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol. Japan; 1971;15:477–81.
Díez-Aguilar M, Ekkelenkamp M, Morosini MI, Merino I, de Dios CJ, Jones M, et al. Antimicrobial susceptibility of non-fermenting Gram-negative pathogens isolated from cystic fibrosis patients. Int J Antimicrob Agents. 2019;53:84–8.
Hansen CR, Pressler T, Nielsen KG, Jensen P, Bjarnsholt T, Høiby N. Inflammation in Achromobacter xylosoxidans infected cystic fibrosis patients. J Cyst Fibros [Internet]. European Cystic Fibrosis Society; 2010;9:51–8. Available from: https://doi.org/10.1016/j.jcf.2009.10.005
Mantovani RP, Levy CE, Yano T. A heat-stable cytotoxic factor produced by Achromobacter xylosoxidans isolated from Brazilian patients with CF is associated with in vitro increased proinflammatory cytokines. J Cyst Fibros [Internet]. European Cystic Fibrosis Society.; 2012;11:305–11. Available from: https://doi.org/10.1016/j.jcf.2012.02.002
Prado MKB, Locachevic GA, Zoccal KF, Paula-Silva FWG, Fontanari C, Ferreira JC, et al. Leukotriene B4 is essential for lung host defence and alpha-defensin-1 production during Achromobacter xylosoxidans infection. Sci Rep. England; 2017;7:17658.
Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science United States. 1998;282:2085–8.
Kawai T, Akira S. The roles of TLRs, RLRs and NLRs in pathogen recognition. Int Immunol England. 2009;21:317–37.
Molinaro A, Holst O, Di LF, Callaghan M, Nurisso A, D’Errico G, et al. Chemistry of lipid a: At the heart of innate immunity. Chem—A Eur J. 2015;21:500–19.
Park BS, Lee J-O. Recognition of lipopolysaccharide pattern by TLR4 complexes. Exp Mol Med. United States; 2013;45:e66.
Wright SD, Ramos RA, Tobias PS, Ulevitch RJ, Mathison JC. CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science United States. 1990;249:1431–3.
Haziot A, Tsuberi BZ, Goyert SM. Neutrophil CD14: biochemical properties and role in the secretion of tumor necrosis factor-alpha in response to lipopolysaccharide. J Immunol United States. 1993;150:5556–65.
Funda DP, Tuckova L, Farre MA, Iwase T, Moro I, Tlaskalova-Hogenova H. CD14 is expressed and released as soluble CD14 by human intestinal epithelial cells in vitro: lipopolysaccharide activation of epithelial cells revisited. Infect Immun. United States; 2001;69:3772–81
Su GL, Dorko K, Strom SC, Nussler AK, Wang SC. CD14 expression and production by human hepatocytes. J Hepatol Netherlands. 1999;31:435–42.
Kim J-I, Lee CJ, Jin MS, Lee C-H, Paik S-G, Lee H, et al. Crystal structure of CD14 and its implications for lipopolysaccharide signaling. J Biol Chem United States. 2005;280:11347–51.
Gregory CD. CD14-dependent clearance of apoptotic cells: relevance to the immune system. Curr Opin Immunol. 2000;12:27–34.
Roncon-Albuquerque RJ, Moreira-Rodrigues M, Faria B, Ferreira AP, Cerqueira C, Lourenco AP, et al. Attenuation of the cardiovascular and metabolic complications of obesity in CD14 knockout mice. Life Sci Netherlands. 2008;83:502–10.
Zoccal KF, Gardinassi LG, Sorgi CA, Meirelles AFG, Bordon KCF, Glezer I, et al. CD36 Shunts Eicosanoid Metabolism to Repress CD14 Licensed Interleukin-1beta Release and Inflammation. Front Immunol. Switzerland; 2018;9:890.
Zoccal KF, Bitencourt C da S, Paula-Silva FWG, Sorgi CA, de Castro Figueiredo Bordon K, Arantes EC, et al. TLR2, TLR4 and CD14 recognize venom-associated molecular patterns from Tityus serrulatus to induce macrophage-derived inflammatory mediators. PLoS One. United States; 2014;9:e88174.
Zanoni I, Granucci F. Role of CD14 in host protection against infections and in metabolism regulation. Front Cell Infect Microbiol. 2013;4:1–6.
de Macedo LH, Souza COS, Gardinassi LG, Faccioli LH. CD14 regulates the metabolomic profiles of distinct macrophage subsets under steady and activated states. Immunobiology. Netherlands; 2022;227:152191.
Haziot A, Ferrero E, Köntgen F, Hijiya N, Yamamoto S, Silver J, et al. Resistance to endotoxin shock and reduced dissemination of gram-negative bacteria in CD14-deficient mice. Immunity. 1996;4:407–14.
Leturcq DJ, Moriarty AM, Talbott G, Winn RK, Martin TR, Ulevitch RJ. Antibodies against CD14 protect primates from endotoxin-induced shock. J Clin Invest. 1996;98:1533–8.
Metkar S, Awasthi S, Denamur E, Kim KS, Gangloff SC, Teichberg S, et al. Role of CD14 in Responses to Clinical Isolates of Escherichia coli: Effects of K1 Capsule Expression. Infect Immun [Internet]. 2007;75:5415 LP – 5424. Available from: http://iai.asm.org/content/75/11/5415.abstract
Anas A, Poll T V.D., de Vos AF. Role of CD14 in lung inflammation and infection. Crit Care. 2010;14.
Lemos MP, McKinney J, Rhee KY. Dispensability of surfactant proteins A and D in immune control of Mycobacterium tuberculosis infection following aerosol challenge of mice. Infect Immun United States. 2011;79:1077–85.
Souza COS, Espíndola MS, Fontanari C, Prado MKB, Frantz FG, Rodrigues V, et al. CD18 Regulates monocyte hematopoiesis and promotes resistance to experimental schistosomiasis. Front Immunol. 2018;9:1970.
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR. Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem United States. 1982;126:131–8.
Paula-Silva FWG, Petean IBF, da Silva LAB, Faccioli LH. Dual role of 5-lipoxygenase in osteoclastogenesis in bacterial-induced apical periodontitis. J Endod United States. 2016;42:447–54.
Wu Z, Zhang Z, Lei Z, Lei P. CD14: Biology and role in the pathogenesis of disease. Cytokine Growth Factor Rev [Internet]. 2019;48:24–31. Available from: https://www.sciencedirect.com/science/article/pii/S1359610119300760
Effah CY, Drokow EK, Agboyibor C, Ding L, He S, Liu S, et al. Neutrophil-Dependent Immunity During Pulmonary Infections and Inflammations. Front Immunol. 2021;12: 689866.
Roy S, Karmakar M, Pearlman E. CD14 mediates Toll-like receptor 4 (TLR4) endocytosis and spleen tyrosine kinase (Syk) and interferon regulatory transcription factor 3 (IRF3) activation in epithelial cells and impairs neutrophil infiltration and Pseudomonas aeruginosa killing in vivo. J Biol Chem United States. 2014;289:1174–82.
Ebong SJ, Goyert SM, Nemzek JA, Kim J, Bolgos GL, Remick DG. Critical role of CD14 for production of proinflammatory cytokines and cytokine inhibitors during sepsis with failure to alter morbidity or mortality. Infect Immun [Internet]. American Society for Microbiology; 2001;69:2099–106. Available from: https://pubmed.ncbi.nlm.nih.gov/11254563
Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med. 2020;2255–73.
Bas S, Gauthier BR, Spenato U, Stingelin S, Gabay C. CD14 Is an Acute-Phase Protein. J Immunol. 2004;172:4470–9.
Gay NJ, Symmons MF, Gangloff M, Bryant CE. Assembly and localization of Toll-like receptor signalling complexes. Nat Publ Gr [Internet]. Nature Publishing Group; 2014;14:546–58. Available from: http://dx.doi.org/https://doi.org/10.1038/nri3713
Janeway CA, Medzhitov R. I Nnate I Mmune R Ecognition. Annu Rev Immunol. 2002;20:197–216.
Qureshi ST, Lariviere L, Leveque G, Clermont S, Moore KJ, Gros P, et al. Endotoxin-tolerant mice have mutations in Toll-like receptor 4 (Tlr4). J Exp Med United States. 1999;189:615–25.
Regueiro V, Campos MA, Morey P, Sauleda J, Agustí AGN, Garmendia J, et al. Lipopolysaccharide-binding protein and CD14 are increased in the bronchoalveolar lavage fluid of smokers. Eur Respir J. 2009;33:273–81.
Virchow JC, Julius P, Matthys H, Kroegel C, Luttmann W. CD14 expression and soluble CD14 after segmental allergen provocation in atopic asthma. Eur Respir J. 1998;11:317–23.
Ayaslioglu E, Tekeli E, Birengel S. Significant elevation of serum soluble CD14 levels in patients with Brucellosis. Jpn J Infect Dis. 2005;58:11–4.
Buchheister S, Buettner M, Basic M, Noack A, Breves G, Buchen B, et al. CD14 Plays a Protective Role in Experimental Inflammatory Bowel Disease by Enhancing Intestinal Barrier Function. Am J Pathol [Internet]. American Society for Investigative Pathology; 2017;187:1106–20. Available from: https://doi.org/10.1016/j.ajpath.2017.01.012
Wenneras C, Ave P, Huerre M, Arondel J, Ulevitch RJ, Mathison JC, et al. Blockade of CD14 increases Shigella-mediated invasion and tissue destruction. J Immunol United States. 2000;164:3214–21.
Furusako S, Takahashi T, Mori S, Takahashi V, Tsuda T, Namba M, et al. Protection of mice from LPS-induced shock by CD14 antisense oligonucleotide. Acta Med Okayama. Acta. Med. Okayama; 2001;55:10.
Wiersinga WJ, Vos AF De, Wieland CW, Leendertse M, Roelofs JJTH, Poll T Van Der. CD14 Impairs Host Defense against Gram-Negative Sepsis Caused by Burkholderia pseudomallei in Mice. 2008;198.
Alarcón-Vila C, Baroja-Mazo A, de Torre-Minguela C, Martínez CM, Martínez-García JJ, Martínez-Banaclocha H, et al. CD14 release induced by P2X7 receptor restricts inflammation and increases survival during sepsis. Elife [Internet]. eLife Sciences Publications, Ltd; 2020;9:e60849. Available from: https://pubmed.ncbi.nlm.nih.gov/33135636
Chakraborty S, Kaur S, Guha S, Batra SK. The multifaceted roles of neutrophil gelatinase associated lipocalin (NGAL) in inflammation and cancer. Biochim Biophys Acta. 2012;1826:129–69.
Knapp S, Wieland CW, Florquin S, Pantophlet R, Dijkshoorn L, Tshimbalanga N, et al. Differential roles of CD14 and Toll-like receptors 4 and 2 in murine Acinetobacter pneumonia. Am J Respir Crit Care Med. 2006;173:122–9.
Wilkinson TS, Dhaliwal K, Hamilton TW, Lipka AF, Farrell L, Davidson DJ, et al. Trappin-2 promotes early clearance of Pseudomonas aeruginosa through CD14-dependent macrophage activation and neutrophil recruitment. Am J Pathol [Internet]. 2009/03/05. American Society for Investigative Pathology; 2009;174:1338–46. Available from: https://pubmed.ncbi.nlm.nih.gov/19264904
Yang S-C, Tsai Y-F, Pan Y-L, Hwang T-L. Understanding the role of neutrophils in acute respiratory distress syndrome. Biomed J [Internet]. 2021;44:439–46. Available from: https://www.sciencedirect.com/science/article/pii/S2319417020301499
Guardado S, Ojeda-Juárez D, Kaul M, Nordgren TM. Comprehensive review of lipocalin 2-mediated effects in lung inflammation. Am J Physiol Cell Mol Physiol [Internet]. American Physiological Society; 2021;321:L726–33. Available from: https://doi.org/10.1152/ajplung.00080.2021
Dessing MC, Knapp S, Florquin S, De Vos AF, Van Der Poll T. CD14 facilitates invasive respiratory tract infection by Streptococcus pneumoniae. Am J Respir Crit Care Med. 2007;175:604–11.
Wieland CW, Van Der Windt GJW, Wiersinga WJ, Florquin S, Van Der Poll T. CD14 contributes to pulmonary inflammation and mortality during murine tuberculosis. Immunology. 2008;125:272–9.
Ciesielska A, Matyjek M, Kwiatkowska K. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cell Mol Life Sci [Internet]. 2021;78:1233–61. Available from: https://doi.org/10.1007/s00018-020-03656-y
Ali A, Tahir R, Shahzad F, Kashif M, Jahan S, Afzal N. Cd14 gene (−159 c>t) polymorphism and its surface expression on monocytes in pulmonary tuberculosis patients. Open Access Maced J Med Sci. 2020;8:203–7.
Lin S-M, Frevert CW, Kajikawa O, Wurfel MM, Ballman K, Mongovin S, et al. Differential regulation of membrane CD14 expression and endotoxin-tolerance in alveolar macrophages. Am J Respir Cell Mol Biol [Internet]. 2004/04/01. 2004;31:162–70. https://pubmed.ncbi.nlm.nih.gov/15059784
Marcos V, Latzin P, Hector A, Sonanini S, Hoffmann F, Lacher M, et al. Expression, regulation and clinical significance of soluble and membrane CD14 receptors in pediatric inflammatory lung diseases. Respir Res. England; 2010;11:32.
Bowman ER, Cameron CMA, Avery A, Gabriel J, Kettelhut A, Hecker M, et al. Levels of Soluble CD14 and tumor necrosis factor receptors 1 and 2 May be predictive of death in severe coronavirus disease 2019. J Infect Dis. 2021;223:805–10.
Landmann R, Link S, Sansano S, Rajacic Z, Zimmerli W. Soluble CD14 activates monocytic cells independently of lipopolysaccharide. Infect Immun. 1998;66:2264–71.
Lévêque M, Le JKS, Jouneau S, Moulis S, Desrues B, Belleguic C, et al. Soluble CD14 acts as a DAMP in human macrophages: Origin and involvement in inflammatory cytokine/chemokine production. FASEB J. 2017;31:1891–902.
Acknowledgements
The authors thank Drª. Joseane Cristina Ferreira, Drª. Viviani Nardini Takahashi, Caroline Fontanari, Elaine Medeiros Floriano, Alyne Fávero Galvão Meirelles, Dr. Carlos Arterio Sorgi and Fabiana Rosseto de Moraes for technical support.
Funding
This work was supported by grants from São Paulo Research Foundation (FAPESP; grant #2014/07125–6), from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, process number: 134209/2017–6 and grant: 303259/2020-5) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Finance Code 001).
Author information
Authors and Affiliations
Contributions
JE-O planned and performed the experiments, analyzed the data, organized the figures and wrote the manuscript. MKBP helped to perform the experiments and reviewing the manuscript. COSS and MRP helped to perform the experiments. SGR and ALCD helped with histopathological analysis and bacterial culture, respectively. LGG helped with the data interpretation and edited the manuscript. LHF conceived and supervised the study, designed the experiments, participated in the data analysis and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Compliance with ethical standards
All experiments carried out in this work were approved by the Ethics Committee on the Use of Animals (CEUA) of Faculdade de Ciências Farmacêuticas de Ribeirão Preto, protocol 17.1.820.60.0.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elias-Oliveira, J., Prado, M.K.B., Souza, C.O.S. et al. CD14 signaling mediates lung immunopathology and mice mortality induced by Achromobacter xylosoxidans. Inflamm. Res. 71, 1535–1546 (2022). https://doi.org/10.1007/s00011-022-01641-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-022-01641-8