Abstract
Stroke is a leading cause of mortality and disability worldwide. In the last couple of decades, improved hyperacute interventions have resulted in improved survival and reduction in severity of subsequent disability in developed countries. Even in developing countries, survival has improved due to better availability of life-sustaining interventions. However, improved survival is resulting in higher number of patients living with significant disability. Therefore, both developed and developing countries are required to provide comprehensive services for stroke, starting from hyperacute care to community and home-based rehabilitation services. There is sufficient evidence to propose establishment of such a continuum. Throughout the continuum, rehabilitation forms an integral component of stroke management plan and must be made available as part of overall stroke care. In this chapter, we provide a comprehensive overview of the stroke care continuum with recommendations for delivery of rehabilitation services to stroke survivors throughout the continuum in the context of both developed and developing countries.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Stroke care has changed from being largely supportive to interventional with emphasis on reduction of both mortality and resultant disability (Schwamm et al. 2005; Powers et al. 2018). The development that started with integrated stroke units has evolved into hyperacute stroke care with emphasis on early diagnosis and revascularization, by either dissolving the clot or mechanically removing it (Marler et al. 2000; Rha and Saver 2007; Higashida et al. 2013; Powers et al. 2018). Alongside the early administration of recombinant tissue plasminogen activator and thrombectomy, one other intervention showing some promise in limiting the long-term disabling impact of stroke is early rehabilitation (Langhorne 2013; Momosaki et al. 2016; Coleman et al. 2017; Yagi et al. 2017). Furthermore, there is now an understanding that establishing a continuum of stroke rehabilitation provides for best possible outcome for stroke patients (NICE 2013). Therefore, it is important to define the service structure for rehabilitation, one that follows the patient through the course of stroke care continuum. This chapter deals with recommendations in this context.
Stroke rehabilitation is a continuous process that starts at the time the patient first presents with impairments and may need to be provided throughout the rest of his or her living years (Teasell et al. 2018). In order to do so, it is imperative that rehabilitation encounters are appropriately defined in terms of timing, service structures and resource requirements. Furthermore, effective interventions at each level of care must also be identified. Based on current evidence, we recommend the following settings as components of the stroke rehabilitation continuum:
-
1.
Early rehabilitation (hyperacute phase and acute phase).
-
2.
Subacute rehabilitation.
-
3.
Outpatient rehabilitation.
-
4.
Home-based rehabilitation.
-
5.
Community-based rehabilitation.
-
6.
Long-term and sustained rehabilitation.
2 Methodological Considerations
We present the current best evidence and evidence-based recommendations for specific interventions addressing each target domain of rehabilitation in stroke patients. As outlined in chapter “Clinical Pathways in Stroke Rehabilitation: Background, Scope, and Methods”, the focus is on best evidence and the corresponding recommendations, but not on explicit health system design prescriptions. Clinical pathways for health system designs depend largely on regional circumstances and have to be developed locally taking both the evidence-based recommendations and the local context and needs into consideration (Platz 2019).
Nevertheless, there is still a need for guidance on health system design for stroke rehabilitation. Whilst we acknowledge the need for regional adaptation of specific practice recommendations and hence have been reluctant to make very explicit recommendations on system design in other chapters, in this chapter, the global author group provides some more general guidance on how to build healthcare settings for stroke rehabilitation.
This chapter makes primarily recommendations on how (best) to organize health care for stroke rehabilitation on a continuum from stroke onset to the long-term situation of living with stroke sequelae. Since we know that such a continuum of care cannot be implemented in many regional settings, this chapter concludes with reflections on how to deal with the contextual limitations that exists in many low-income countries or rural settings. These limitations often include a severe shortage of trained staff and even most basic rehabilitative interventions often rely on the dedication of family members or other volunteers (see Sect. 3.7 for discussion).
In contrast to specific interventions, there is paucity of evidence addressing benefit, harm and cost-effectiveness of healthcare settings. Therefore, this chapter is largely based on clinical reasoning and experience from clinical practice in diverse settings ranging from low-income to high-income countries. Many recommendations made are expert opinions. When evidence is available, this is referenced and the level of evidence is then categorized according to the Oxford Centre for Evidence-Based Medicine—Levels of Evidence and rated with four categories according to “GRADE” (“Grades of Recommendation, Assessment, Development and Evaluation”) (Owens et al. 2010):
-
High quality: further research is unlikely to affect our confidence in the estimation of the (therapeutic) effect.
-
Medium quality: further research is likely to affect our confidence in the estimation of the (therapeutic) effect and may alter the estimate.
-
Low quality: further research will most likely influence our confidence in the estimation of the (therapeutic) effect and will probably change the estimate.
-
Very low quality: any estimation of the (therapy) effect or prognosis is very uncertain.
Whenever possible, recommendations of existing guidelines and/or evidence-based reviews have been included.
3 Stroke Rehabilitation Continuum
3.1 Early Rehabilitation After Stoke
With reduction in stroke mortality (Seminog et al. 2019) and more patients surviving the acute phase, attention is now focused on reduction of morbidity and disability due to stroke. Revascularization with tPA or mechanical thrombectomy as well as protection of neural tissue by effective management of complications, such as haemorrhagic transformation of infarct or brain oedema, is directed at limiting the extent of brain damage and thereby the disabling effect of impairments. To support this effort, emphasis on recovery of function and prevention of secondary complications should be considered as the main goal of early rehabilitation (Winstein et al. 2016). When rehabilitation is provided in an intensive care setting immediately after stroke, it is best referred to as hyperacute, whilst ward-based or step-down unit level rehabilitation should be termed as acute rehabilitation. Early rehabilitation refers to both of these levels of care. It is advisable, however, to use the individual terms as these reflect the exact level of rehabilitation setting more distinctly. The provision for early rehabilitation is recommended in the American Heart Association Guidelines, with evidence for this recommendation graded at 1A (Winstein et al. 2016) corresponding to a strong recommendation (A) building on high-quality evidence.
In hyperacute setting, the stroke care team ought to include at least a physician with expertise in stroke rehabilitation, speech and language pathologist/therapist with expertise in swallow and early communication techniques, physical therapist, occupational therapist and stroke care–trained nurse specialists (Boulanger et al. 2018). In this setting, the main goal of rehabilitation should be to prevent early complications and assess safety and feasibility of early mobilization (Coleman et al. 2017). In this context the key domains of care are:
-
1.
Complete assessment of patient with focus on the following:
-
(a)
Impact of stroke with particular focus on presenting impairments and their severity (impairment mapping).
-
(b)
Co-morbidities and their premorbid impact on function.
-
(c)
Pre-existing musculoskeletal conditions and/or deformities.
-
(d)
Pre-existing disability(ies).
-
(e)
Family setup and support.
-
(f)
Work and social status.
-
(a)
-
2.
Protection of the airway and swallow assessment and management.
-
(a)
Early swallow assessment by speech and language therapist, who is adequately trained in dysphagia management or by another professional (nurse or doctor), is recommended (Palli et al. 2017). Although, as yet, evidence is not conclusive regarding efficacy of this practice in reducing the aspiration episodes (Smith et al. 2018), it is strongly recommended that screening should be carried out (Wolfe and Rudd 2011; Lakshminarayan et al. 2010) and in our judgement it should be adopted as part of acute stroke care.
-
(b)
The patient should not be fed orally or given medications unless cleared by swallow screening (Duncan et al. 2005).
-
(c)
The period within which this is to be conducted is difficult to specify as evidence in this respect does not support a standardized practice. However, currently, there is a consensus agreement that in patients who have signs of dysphagia, the assessment should be carried out within 24 h (Ellis and Adams 2016).
-
(d)
At present, there is no consensus on the instrument or instruments for the assessment, and we recommend that this should be agreed upon locally depending on resources, needs, availability, expertise and training (Donovan et al. 2013).
-
(e)
Enteral feeding should be initiated early in patients with dysphagia to avoid malnourishment. Whilst this should be considered as early as it is clinically established that patient is not able to swallow, the delay in introducing the enteral feeding should not exceed 3 days (Yamada 2015; Ojo and Brooke 2016).
-
(f)
Evidence indicate that early insertion of per-endoscopic gastrostomy tube should be avoided (George et al. 2017).
-
(g)
In patients requiring enteral feeding, nasogastric tube feeding is recommended for as long as 3 weeks, beyond which insertion of PEG may be considered (George et al. 2017). Please note that nasogastric tube feeding can be associated with regurgitation and aspiration if the patient lies down immediately after a meal. Therefore, the patient should remain seated for over 2 h (gastric emptying time) after each meal to avoid regurgitation and aspiration.
-
(a)
-
3.
Very early or early mobilization (VEM/EM):
-
(a)
Currently, there is no evidence to support VEM (defined as out of bed activity within 24–48 h). Indeed, AVERT III showed negative impact on mortality at 3 months (Langhorne et al. 2018; Bernhardt et al. 2019).
-
In the light of lack of evidence for beneficial effect and evidence for negative impact at 3 months, we recommend that mobilization within 24 h after stroke cannot be recommended (Langhorne et al. 2018).
-
Mobilization within 48 h may be considered acceptable in patients who meet key safety parameters. However, there is still no convincing evidence for efficacy of this practice (Xu et al. 2017).
-
-
(b)
Early mobilization is recommended.
-
Currently there is no agreement on the definition of “EARLY”. Mobilization within 72 h may be considered as such (Bernhardt et al. 2015).
-
On the basis of current evidence, mobilization after 24 h, unless otherwise contraindicated, is recommended. There are no studies to indicate that this practice is likely to harm patient and indeed, there is some evidence that it may be of some benefit (Li et al. 2018).
-
Dose, including intensity, frequency and duration should be commensurate to patient’s clinical status. Dose should be incrementally increased in line with patient’s tolerance and response (Yagi et al. 2017).
-
Specific motor rehabilitation focuses are head and trunk control, arm function, stance, gait and balance and should be addressed as individually indicated early after stroke.
-
Change, progress and outcome should be analytically recorded daily.
-
-
(a)
-
4.
Communication and speech.
-
(a)
Early assessment of communication by a speech therapist is recommended.
-
(b)
Strategies for establishing communication early with stroke patients are recommended (National Institute for Health and Care Excellence (NICE) 2013).
-
(c)
The evidence for active speech and language therapy in early period after stroke, before 48 h, is not available (Nouwens et al. 2013).
-
(d)
There is some evidence that speech and language therapy when commenced from 2 days onwards has a beneficial effect on outcome (Mattioli et al. 2014). It is therefore, good practice to commence active speech and language therapy from 48 h onwards for dysphasic/aphasic patients.
-
(a)
-
5.
Sensory and perceptual deficits.
-
(a)
Early detection of sensory and perceptual deficits is recommended.
-
(b)
There is evidence for introducing rehabilitation strategies for sensory deficit in early stroke rehabilitation (Pandian et al. 2014).
-
(c)
Given the current evidence, it is recommended that patients who are able to comprehend presence of deficits such as somatosensory deficits, visual field deficits, hemi-neglect or visual inattention should be made aware of these and rehabilitation strategies should be introduced early.
-
(a)
3.1.1 Prevention of Secondary Complications
An important role of rehabilitation team in early rehabilitation is prevention of complications. This has now been highlighted as key responsibility of rehabilitation teams in hyperacute and acute rehabilitation settings (Winstein et al. 2016).
The rehabilitation team must take steps to prevent, rapidly detect and treat
-
Malnutrition and dehydration.
-
Pressure sores.
-
Aspiration-related chest infections.
-
Over dependence on ancillary devices such as urinary catheter, tracheostomy tube and feeding tube.
-
Contractures.
-
Excessive muscle wasting.
-
Shoulder pain and positional malalignment.
-
Agitation and restlessness.
-
Mood disorder/depression and social isolation.
-
Urinary tract infection.
3.2 Subacute Stroke Rehabilitation
Subacute stroke rehabilitation is the next level of care for stroke patients. As shown for many of the target domains in this book and in national guidelines, in the subacute stage of stroke, interventions should be intensive, challenging and tailored towards the individual needs of the patients.
When a patient is deemed fit to be discharged or transferred from acute care, a decision has to be made by the treating team whether a safe discharge home is possible or the patient should be transferred to a specialized facility to continue structured multidisciplinary stroke rehabilitation. Subacute stroke rehabilitation units are either stand-alone services or may be part of larger acute care hospitals. There is some evidence in favour of this level of care of stroke patients (Rønning and Guldvog 1998). Several factors influence this decision: These include:
-
Availability of required subacute stroke rehabilitation facilities (currently only developed healthcare systems consistently provide this level of care).
-
Affordability of subacute rehabilitation.
-
State funded (most are eligible, but waiting lists and duration may be barriers).
-
Medical insurance (restrictive/selective).
-
Self-funding (expensive).
-
Charity funding (limited).
-
-
Geographical location and accessibility to patient and his or her family.
-
Medical capability of a facility, as this determines at what stage patient may be transferred. For example, if the patient has a tracheostomy tube and subacute rehabilitation facility that he or she can be transferred to does not have a clinical set up to cater for tracheostomized patients then a safe transfer is not possible. This results in longer stay in acute care with limited access to subacute level of rehabilitation.
3.2.1 Transfer Criteria to Subacute Rehabilitation Facility
Whilst transfer criteria will differ from place to place and will depend on the services available at the subacute rehabilitation facility, some guiding criteria for transfer from acute to subacute level of rehabilitation may be applied:
-
1.
All investigations required for determining the nature and cause of stroke have been completed.
-
2.
All required interventions for secondary preventions have been optimized.
-
3.
Medical stability has been achieved with satisfactory control of blood pressure and diabetes mellitus.
-
4.
Patient continues to need close physician supervision.
-
5.
Patient continues to need specialized nursing care.
-
6.
Patient is cognitively able to engage meaningfully in therapies.
-
7.
Patient is able to tolerate higher intensity of therapies.
-
8.
Patient requires more than one therapy input daily.
-
9.
Patient and family have been suitably counselled to accept lesser level of medical surveillance and higher intensity of rehabilitation.
-
10.
Patient and family have agreed to the transfer and fully understand its need.
3.2.2 Subacute Rehabilitation Facility
The subacute rehabilitation facility for stroke patients should have integrated multidisciplinary set up for provision of this level of rehabilitation. The patient should be offered intensive therapies. We recommend that for optimal functioning a facility should at least meet the following standards:
-
The physical space and environment should be optimal and conducive to adequately accommodate the number of patients a given facility is likely to serve.
-
The multidisciplinary team should include the following categories of staff:
-
Physician(s) with expertise in neurorehabilitation.
-
Rehabilitation-trained nurses.
-
Neurological physical therapists.
-
Neurological occupational therapists.
-
Neurological speech and language therapist with expertise in dysphagia management and communication rehabilitation.
-
Dietician(s).
-
Social worker(s)/case manager(s).
-
-
When available, the provision of neuropsychological and orthoptic services is recommended.
The facility should have links with or access to orthotic, neurological, urological, psychiatry, ophthalmology and general medical services.
-
The facility should have all essential therapy equipment and aids.
-
The facility should have dedicated therapy areas, e.g. for physiotherapy, occupational therapy and speech and language therapy.
-
Social networking spaces and provision for community re-integration (shopping, leisure trips, etc.) are desirable.
The ideal staff to patient ratios have not been optimally evaluated and differ in various settings. We recommend that the following ratios be considered for planning such facilities:
-
One physician (with expertise in neurorehabilitation) should not be expected to supervise the care of more than 20–25 inpatients.
-
Nurse to patient ratio: No more than 5 patients to one nurse.
-
Physiotherapist to patient ratio: No more than 10 patients to one physiotherapist.
-
Occupational therapist to patient ratio: No more than 10 patients to one occupational therapist.
-
Speech and language therapist to patient ratio: No more than 20 patients to one speech and language therapist.
-
For each 40 patients one neuropsychologist is recommended.
3.2.3 The Transfer Process
The representative of the subacute rehabilitation facility should meet with patient and his or her family ahead of transfer and fully brief them about the nature of services offered and the level of care they should expect. The transfer process should also be clearly explained.
The transfer process should be well coordinated and adjusted to the patient’s needs. The following standards should be adhered to:
-
All required documentation including discharge summaries from each discipline involved in the care of the patient in the referring facility should be provided to the subacute rehabilitation facility.
-
The discharge medications complete with doses and schedules should be clearly listed.
-
Detailed nursing handover should be provided.
-
All required equipment and devices (e.g. orthosis, splints, wheelchair) necessary for continued care of the patient should be provided.
3.2.4 Subacute Rehabilitation Programmes
After admission, the patient should have structured care provided to him or her. The facility should have standardized policies for all sessions and domains of care. These include:
-
Mobility training including gait training and where necessary training for full or semi-independence from wheelchair.
-
Management of cognitive impairment and cognitive rehabilitation.
-
Management of perceptual deficits.
-
Management of dysphagia with the aim of retraining for oral feeding where this is possible to do safely.
-
Participation in activities of daily living.
-
Neuropathic pain management.
-
Spasticity management.
-
Management of mood disorder.
-
Adjustment and “beginning to live with disability” training.
-
Readiness for discharge to home or modified living.
The policies should highlight minimum standard of care for each domain of care. There should be agreed timeline for initial assessments and care planning and goals set thereafter should be measurable and achievable in realistic time frame. The following are some guiding parameters in this context:
-
Patient(s) should undergo full multidisciplinary team (MDT) assessment within 24–72 h of admission.
-
The MDT should develop a goal-directed care plan with specified timelines.
-
The patient and family should be fully briefed about the care plan and their suggestions and concerns taken into consideration and the care plan adjusted accordingly.
-
The progress of the patient should be reviewed by the MDT at least every week and goals and care plan modified to adjust for change.
-
Discharge planning should start early, preferably within 1 week of admission.
-
Periodic patient and family meetings should be held to brief them about the progress.
Discharge planning meeting must always be convened.
The aim of subacute rehabilitation is to achieve clinical stability and functional readiness for discharge to community, home or modified living facility. This entails gaining modified partial to full independence and predictability of care needs. The discharge should be appropriately planned and the patient should be transferred to either outpatient or home-based rehabilitation services.
The specific recommendations given above have been formulated on the basis of good practice and in line with those detailed in several existing guidelines (Winstein et al. 2016; Gittler and Davis 2018).
The overall evidence for the effectiveness of this level of rehabilitation is not robust for the whole group of stroke patients (García-Rudolph et al. 2019). Teasell and co-workers differentiated their analysis according to the severity of stroke (Teasell et al. 2018; evidence-based review of stroke rehabilitation):
-
In mildly affected patients, the site of rehabilitation does not influence functional outcome (level of evidence 1A; high-quality evidence),
-
For the subgroup of patients with moderately severe stroke, specialized rehabilitation in a subacute rehabilitation unit does improve functional outcome compared to conventional care on a general ward (level of evidence 1A; high-quality evidence),
-
Patients with severe or moderately severe stroke who receive treatment on a stroke rehabilitation unit have a lower risk of being dependent or dead/dependent compared with patients who receive little or no rehabilitation (level of evidence 1B; medium-quality evidence).
Not all patients will need treatment within a special subacute rehabilitation facility. Especially patients with mild or moderate functional deficits may prefer to attend specific rehabilitation modules on an outpatient basis or even at home using tele-therapeutic devices (see also Sect. 3.6).
3.3 Outpatient Stroke Rehabilitation Services
Patients may be discharged from acute care and subacute facilities with arrangement to receive ongoing rehabilitation as outpatients. Indeed, there is evidence that early supported discharge directly from acute care to community-based rehabilitation as well as integrated outpatient rehabilitation delivers good outcome for stroke survivors (Rice et al. 2016; Langhorne et al. 2017). Teasell et al. (2018) found level 1A evidence that stroke patients with mild-to-moderate disability, discharged early from an acute hospital unit, can be rehabilitated in the community by an interdisciplinary stroke rehabilitation team and attain similar or superior functional outcomes when compared to patients receiving inpatient rehabilitation (high-quality evidence).
The patient could be referred to an outpatient stroke rehabilitation service if:
-
He/she is clinically stable and is able to tolerate transportation to and from outpatient rehabilitation facility.
-
He/she has sufficient effort tolerance level and does not fatigue so much that precludes effective participation in therapy sessions.
-
He/she is able to engage cognitively in therapy sessions, re-engage in subsequent sessions with demonstrable carry over.
The outpatient stroke rehabilitation facility should be designed to offer multidisciplinary team rehabilitation. Patients should have access to all required therapies and interventions. The available services should include:
-
Access to physician(s) with expertise in neurorehabilitation for continued management of residual effects of stroke including spasticity and pain.
-
Physiotherapy service with adequately designed treatment areas with availability of most required equipment.
-
Occupational therapy service with capacity to attend to issues such as extended activities of daily living and vocational rehabilitation.
-
Speech and language therapy services with capacity to work on issues related to dysphagia and communication.
-
Neuropsychological therapy for the treatment of cognitive, behavioural and emotional post-stroke disorders is recommended when available.
-
Optional or ancillary services include dietetics, orthotics and specialized nursing service particularly, continence management. These services may also be accessed through a referral arrangement.
If the patient is able to travel to and from the clinic and logistically it is possible to do so with the least level of disruption to family life, then outpatient rehabilitation is preferable to home-based rehabilitation. In less developed healthcare systems, cost and availability may limit access and this may be combined/supplemented with home-based rehabilitation.
3.4 Home-Based (Family-Based) Stroke Rehabilitation
Once patients with stroke have been discharged home, it is important to continue with rehabilitation. Home-based rehabilitation in the present context is defined as a form of rehabilitation, where the training is provided by members of the family. It may be beneficial as it realizes the actual need-based training true to the patient’s living environment. Task shifting is an attractive solution for healthcare sustainability. The patient’s family can be trained to provide task-based training, and members of the rehabilitation team can visit the patient at home as needed to provide required therapies. In low- and middle-income healthcare systems, this may be an effective way of providing ongoing rehabilitation. (Lindley et al. 2017), and the outcomes may be comparable to long-term rehabilitation in non-domiciliary facilities (Mayo 2016). However, home-based (family-based) rehabilitation is under stress where the joint families are disintegrating into nuclear families thereby shrinking the pool of family members who can attend to the rehabilitation of patient after stroke. Therefore, task shifting to family members may increase caregiving burden and stress. Nevertheless, family participation at home reduces the need for travelling for outpatient appointments in centres, especially when distant from patients’ homes. Furthermore, the financial burden is lessened if therapists are not required to administer therapy at home and day-to-day life is not severely disrupted. This may contribute to reduction in patient’s and caregiver’s anxiety and improve quality of life of affected family. Conversely, though it can be argued that in patients with limited functional improvement, over long period of time, the situation may become burdensome and result in caregiver’s fatigue (Sarı 2017).
Furthermore, the results of the ATTEND trial did not demonstrate any benefit of family-led domiciliary care (ATTEND Collaborative Group 2017). This is also consistent with the absence of benefit seen in a systematic review of trials of caregiver-mediated exercises to improve activities of daily living after stroke (Vloothuis et al. 2016). Overall, these findings do not support investment in new stroke rehabilitation services that shift tasks to family caregivers, unless new evidence emerges. (Level 2B evidence, moderate evidence against the establishment of new family-led therapeutic interventions without concomitant research.)
The absence of benefit of the family-rehabilitation intervention has important implications for stroke recovery research, behavioural change, and task shifting in general. A future avenue of research should be to investigate the effects of task shifting to healthcare assistants or team-based community care to offer care after discharge (ATTEND Collaborative Group 2017). Another option may be to combine family-led rehabilitation with outpatient care. This may help reduce the frequency of outpatient care required thus promoting affordability.
3.5 Community-Based Stroke Rehabilitation (CBR)
Over the last couple of decades, CBR has acquired a lot of interest. CBR programmes improve, facilitate, stimulate and/or provide services to people with disabilities (PWDs), such as stroke survivors, their families and caregivers within the locations of their families and communities through locally employed full or part time, paid or volunteer community rehabilitation workers, who are trained, followed up and managed within a certain organizational set up, that has rehabilitation philosophy as its core operational principle (Ru et al. 2017). Only few studies are available on CBR and its advantages and disadvantages have not been critically studied (Stephenson and Wiles 2000). However, it is possible to list some advantages on the basis of experience and current practice.
Advantages of CBR, compared to the institutional approach include:
-
In time, and in theory, all the people living with disabilities in a community can be reached and their basic needs be met.
-
“Tailor-made” rehabilitation programmes can be established, based on the individual’s capacities and needs, and focused directly on integration into the family/community. “Disability” is not a stable situation. CBR can evolve and adapt to changing needs of patients.
-
Family members can witness and participate in the progress of a relative living with disability, thus enhancing their faith in that person’s abilities and potential and challenging their own prejudices.
-
CBR services, apart from carrying out their core work in rehabilitation, can also contribute towards the prevention of secondary complications related to impairments and disabilities, through activities such as primary healthcare, vaccinations, nutrition and hygiene.
-
CBR programmes can trace many people living with disabilities who would never have been found by institutions and, through referral, can make the work of other existing specialized services more effective.
-
CBR can be more effective in tackling issues such as return to work and community access, including leisure activities and extended activities of daily living.
-
CBR could be cost-effective (if well managed!).
Problems of CBR, compared to the institutional-based approach,
-
The poor living conditions of most people with disabilities are also poor conditions for rehabilitation. The objectives of individual CBR programmes therefore have to be very realistic and must focus on essential needs.
-
Community- and home-based services by community rehabilitation workers can sometimes be rather routine and boring, for the worker, client and family alike; this may be less challenging than training or education in a centre.
-
Poor families’ priorities may be at the level of survival rather than solving problems of a member with disability. Furthermore, the disability of one family member is not always problematic for other family members; therefore, it is sometimes very hard to enlist their active collaboration.
-
The organization and management of CBR are complex and difficult due to organizational and political reasons and local priorities for funding.
-
The educational level of the community rehabilitation workers (CRWs) may be low. Better-educated individuals are often difficult to engage in CBR work. Front-line CBR is a low-profile job, which does not offer notable social status to people with higher education.
These factors influence the type, level and quality of the services which can be provided at the community level through a CBR programme. Although, these factors have been determined through critical appraisal of the existing services, there are limited number of studies and it is difficult to provide firm structural basis for community rehabilitation.
In Europe (defined geographically), such structures are already implemented in some countries, e.g. in the UK and in France. As part of the NHS (e.g. in Milton Keynes), Stroke Clinical Specialists are available “to provide in-depth knowledge and expertise; consistent education, support and advice in accessing information and a full range of services from the NHS, social care and others. This service is available to people who have had a stroke/TIA, their relatives and carers, members of the general public, professionals and voluntary organisations” (NHS homepage Milton Keynes, accessed 28.12.2019).
In Germany, pilot studies are run to employ community rehabilitation workers (e.g. “Schlaganfall-Lotsen”) by regional stroke associations (e.g. “Schlaganfall Allianz Sachsen-Anhalt”) or by charities (e.g. “Stiftung Deutsche Schlaganfall-Hilfe”). Their main aims are to provide advice to patients and their relatives, to help to implement elements of effective secondary prevention and help to organize the continuum of stroke care and therapy after discharge from the primary hospital. Similar services are also available or in preparation in other European countries, in some American, Asian and African countries and well established in some areas of Canada and Australia.
The aim of these coordinators is always to guide and to augment the existing structures in the community, they cannot—and should not—substitute the existing medical and therapeutic resources.
In many countries, stroke support groups and stroke survivor organizations (e.g. the Stroke Alliance for Europe (SAFE), a non-profit–making organisation with members from 24 countries) support education and stroke research; they campaign to support the acute treatment and prevention of stroke and help to improve the quality of life of stroke survivors, their families and caretakers.
It is our recommendation that at this time, local realities and resources should determine the structure and extent of services that are possible to provide under this umbrella taking into account the specificities of government run, insurance governed and privately financed systems. In this way, rehabilitation centres can also be included into the structure as local and/or regional centres of excellence especially for more severely affected patients. Such an approach is likely to be useful in low-, middle- and high-income countries. If implemented its effect should be scientifically evaluated whenever possible.
3.6 Long-Term and Sustained Rehabilitation
A significant number of stroke patients survive with established disability and with age as well as ongoing comorbidities. The burden of disability often increases and results in significant loss of function and independence (Meyer et al. 2015). If left unattended, the burden of care may progressively escalate (Van De Port et al. 2006). This can result in loss of employment, social restriction, care providers fatigue as well as ever-increasing financial burden. To date, there is no consensus as to how to support or provide care for stroke survivors in the long term (Aziz et al. 2016). It is, however, important to establish a suitable network of surveillance in order to prevent decline in stroke survivor’s functional status and level of participation over time.
It is recommended that there should be a long-term care support and sustained rehabilitation program for patients with stroke. We recommend that consideration be given to providing this via primary care centres in the community or delivered by a specialist nurse practitioner. In developing and less-developed healthcare systems, a model of care can be developed whereby trained community workers can maintain regular contact with patients and their families and advise them to request help when they deem this is necessary. Modern technology can also be utilized for this purpose and contact can be maintained with patients and their families via mobile phones or specially developed apps. Telemedicine is also being utilized for surveillance (Sarfo et al. 2018) and it is anticipated that this model of care is likely to become widely used for provision of long-term support and sustained rehabilitation for stroke survivors in future.
3.7 Adapting Clinical Pathways to Diverse Regional Healthcare System Contexts
More than 80% of the world’s population live in over 100 developing countries. Delivery of neurologic care in developing countries varies depending on the needs and resources of the country and the availability of medical and paramedical personnel (WHO 2014). Medical insurance and government support are usually minimal or totally lacking. The financial burden is heavy and includes direct costs of inpatient care, outpatient care and therapy sessions, investigations, medications and transport (patients from rural areas often have to travel long distances to urban healthcare centres). The indirect cost includes the loss of earnings due to unemployment during illness and convalescence. In the large majority of these countries, there may be no access to financial support such as disability benefits (Disability and Development Report 2018; Singh 2013).
The availability of neurorehabilitation services is inconsistent and may range from highly sophisticated in developed countries to totally inadequate or lacking in developing and underdeveloped countries. Over 60% of the developing countries have no neurorehabilitation services. There is severe paucity of trained professionals. The task of managing patients with neurological impairments is often devolved to generic therapists and inadequately trained nursing and medical staff. The overall effect is that treatments are being provided by less than adequate professionals, possibly delivering outcomes for patients that fall short of their potential. Even in those developing countries, where some neurorehabilitation service is provided, the quality is rarely good enough due to a lack of a well-structured neurorehabilitation system which can provide comprehensive rehabilitation services. More often than not treatment is not provided (WFNR 2015).
As stated before, hospital-based interdisciplinary neurorehabilitation care should be provided as a first line service to facilitate rapid recovery after neurological injury. The home-based or community-based services are appropriate for settlement at home and community re-integration in the recovery phase. Community-based rehabilitation services are the most appropriate way forward in enhancing outcomes particularly in developing countries, with tailored and culturally sensitive education for the family, to help them participate in the rehabilitation of the patient (Pandian et al. 2015). There have been repeated concerns about the adequacy of the evidence-base regarding the efficacy, effectiveness and efficiency of CBR predominantly using local resource in the local community (Surya 2010, 2015). However, on balance, in developing countries, CBR may be one of the most effective ways of providing rehabilitation after the acute/subacute phase, especially when there is an intimate social system and family structure that helps to provide the necessary physical, emotional and spiritual support. Strong family bond helps to overcome the negative impact of the disability and large extended family system ensures that the physical, social and financial burden of disease is shared.
The role as therapy giver can be switched depending on the availability of family members. Even though, the ATTEND trial ( 2017) and the Cochrane review by Vloothuis et al. (2016) have not shown a clear-cut beneficial effect of (additional) therapy provided by family members, these family members are often the only people available to the patients. They provide valuable social, emotional and psychological support. In order to strengthen and improve their role in delivering rehabilitation, different models for training can be tried to ensure best possible outcomes. As many family members as possible can be trained by the therapist or through web-based teaching application. Use of mobile phone to record the exercises and progress and sharing with the patient/caregiver is useful as patients/caregivers can review them regularly at home to be implemented at home. Mobile phone records of exercises at home also make it possible for therapists to check whether family members are correctly following the programmes at home. The recorded exercise pattern on phone can be reviewed during outpatient visits and any modification or adjustment to the programme can be made. This application is most useful tool in family-based rehabilitation (Zhou et al. 2018).
Family-based and community-based rehabilitation settings are likely to become important models in future for delivery of rehabilitation after the acute/subacute phase of stroke not only in low- and middle-income countries but also in high-income countries. As telemedicine and technologies become more sophisticated, this form of rehabilitation will play a pivotal role in patient’s recovery and improving outcomes.
4 Conclusions
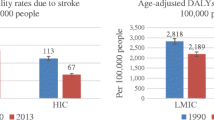
Stroke care has advanced in the past two decades and more patients are surviving the acute stage. The mortality rates are reducing both in developed and developing countries, thereby resulting in increased disability burden (Feigin et al. 2019). In stroke care model, rehabilitation is now considered an integral component of all levels of stroke care (Fig. 1). Whereas, there may be a reduction in the individual level of disability in sophisticated healthcare systems due to timely interventions and reduction of the impact of disabling impairment because of appropriate level of rehabilitative care (Lees et al. 2016; Emberson et al. 2014; Campbell et al. 2015); in developing countries, prolonged survival is associated with heavier burden of disability. The continuum of stroke care, including the pillars of the stroke quadrangle (surveillance, prevention, acute care and rehabilitation), is lacking at many levels and contributes to poor outcome in the developing countries. It is imperative that despite the limitations of resources, appropriate efforts are made to improve services for stroke survivors and foundations are laid upon which an effective continuum of care can be developed. Some low-cost and simple measures can be put in place.
For developed countries, we recommend that the stroke care continuum should be reinforced with mechanisms in place for continual appraisal and improvement. A major challenge foreseen is the increasing demand for stroke rehabilitation that has to be met due to demographic changes with a higher proportion of elderly citizens who are at risk for cerebrovascular accidents.
For developing countries, we recommend that given the current evidence, early mobility, after 24 h, should be encouraged. Intensive care and acute care staff should be educated to pursue this objective. A simple measure of prescribing bed rest beyond 24 h only for those who require it and considering this as an exception may help to improve outcome. Deployment of physical therapists and other therapists in a multidisciplinary setting in hyperacute and acute care services must be considered vital. Training of all nursing staff in moving, handling and positioning of patients should be made mandatory. Furthermore, prevention of secondary complications must be diligently pursued (Scottish Intercollegiate Guidelines Network 2010). In fact, the healthcare cost savings through minimizing secondary complications should pay for any extra resource required to achieve this objective.
In the continuum of stroke care, subacute rehabilitation may be provided by specialized therapists on an outpatient or inpatient basis or in families in private homes, where most of the therapy will be provided by lay persons (Fig. 2). Although intensive and at the same time specific professional therapy after stroke is highly recommended in the subacute phase after stroke (see above), intermediate rehabilitation facilities may be difficult to provide in developing countries due to the cost of setting up and maintaining such facilities. However, where available, such facilities may also support community-based and family-based care by proving oversight and outpatient/inpatient multidisciplinary care as may be needed (see above).
We recommend the development of services in the community with investment in CBR and home-based rehabilitation, utilizing low-cost resources and—building on positive and negative conceptual experience—engaging family members as part of rehabilitation team not only in the subacute stage after stroke but also for long-term and sustained rehabilitation. To incorporate therapy into daily routine and practice is however an unsolved problem—both in developed and developing countries.
We have deliberately avoided explicit recommendations for technical rehabilitation interventions such as robotics, neuromodulation and other such expensive techniques and equipment which due to lack of availability and cost are difficult to generally recommend as necessary for rehabilitation. Furthermore, with regard to recovery of function, the principles of functional brain recovery apply to both technology- and mankind-supported restorative treatment and training. Both approaches or their combination can be recommended based on their regional availability. Both feasibility and cost-effectiveness of purely therapist-led and technology-based rehabilitation vary according to regional socioeconomic circumstances and thus any hitherto decisions have to rest on their regional assessment.
Finally, it is our opinion that all healthcare systems, globally, must make stroke a priority and consider investing in continuum of care for stroke as doing so will result in lesser burden of care in the long-term and may indeed deliver net cost savings.
References
ATTEND Collaborative Group (2017) Family-led rehabilitation after stroke in India (ATTEND): a randomised controlled trial. Lancet 390(10094):588–599 . Epub 2017 Jun 27. https://doi.org/10.1016/S0140-6736(17)31447-2
Aziz NA, Pindus DM, Mullis R, Walter FM, Mant J (2016) Understanding stroke survivors’ and informal carers’ experiences of and need for primary care and community health services—a systematic review of the qualitative literature: protocol. BMJ Open 6(1):e009244. https://doi.org/10.1136/bmjopen-2015-009244
Bernhardt J et al (2015) Early mobilization after stroke: early adoption but limited evidence. Stroke 46(4):1141–1146. https://doi.org/10.1161/STROKEAHA.114.007434
Bernhardt J et al (2019) Very early versus delayed mobilization after stroke. Stroke 50:e178–e179. https://doi.org/10.1161/STROKEAHA.119.024502
Boulanger JM et al (2018) Canadian stroke best practice recommendations for acute stroke management: prehospital, emergency department, and acute inpatient stroke care, 6th edition, update 2018. Int J Stroke 13(9):949–984. https://doi.org/10.1177/1747493018786616
Campbell BCV, Donnan GA, Lees KR, Hacke W, Khatri P, Hill MD et al (2015) Endovascular stent thrombectomy: the new standard of care for large vessel ischaemic stroke. Lancet Neurol 14(8):846–854. https://doi.org/10.1016/S1474-4422(15)00140-4
Coleman ER et al (2017) Early rehabilitation after stroke: a narrative review. Curr Atheroscler Rep 19(12):59. https://doi.org/10.1007/s11883-017-0686-6
Disability and Development Report (2018) Realizing the sustainable development goals for persons with disabilities. https://doi.org/10.18356/6b539901-en
Donovan NJ et al (2013) Dysphagia screening: state of the art invitational conference proceeding from the state-of-the-art nursing symposium, international stroke conference 2012. Stroke 44(4):e24–e31. https://doi.org/10.1161/STR.0b013e3182877f57
Duncan PW et al (2005) Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke 36(9):e100–e143
Ellis C, Adams RJ (2016) Improving stroke outcomes: a roadmap of care. Int J Neurorehabil 3:3. https://doi.org/10.4172/2376-0281.1000215
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E et al (2014) Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384(9958):1929–1935. https://doi.org/10.1016/S0140-6736(14)60584-5
Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N et al (2019) Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(4):459–480. https://doi.org/10.1016/S1474-4422(18)30499-X
García-Rudolph A, Sánchez-Pinsach D, Salleras E, Tormos J (2019) Subacute stroke physical rehabilitation evidence in activities of daily living outcomes: a systematic review of meta-analyses of randomized controlled trials. Medicine 98:e14501. https://doi.org/10.1097/MD.0000000000014501
George BP et al (2017) Timing of percutaneous endoscopic gastrostomy for acute ischemic stroke. Stroke 48(2):420–427. https://doi.org/10.1161/strokeaha.116.015119
Gittler M, Davis AM (2018) Guidelines for adult stroke rehabilitation and recovery. JAMA 319:820. https://doi.org/10.1001/jama.2017.22036
Higashida R et al (2013) Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke 44(10):2961–2984. https://doi.org/10.1161/STR.0b013e3182a6d2b2
Lakshminarayan K et al (2010) Utility of dysphagia screening results in predicting poststroke pneumonia. Stroke 41(12):2849–2854. https://doi.org/10.1161/STROKEAHA.110.597039
Langhorne P (2013) Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev (4):CD000197. https://doi.org/10.1002/14651858.CD000197.pub3
Langhorne P, Baylan S, Trialists ESD (2017) Early supported discharge services for people with acute stroke. Cochrane Database Syst Rev 7(7):CD000443. https://doi.org/10.1002/14651858.CD000443.pub4
Langhorne P et al (2018) Very early versus delayed mobilisation after stroke. Cochrane Database Syst Rev (10):CD006187. https://doi.org/10.1002/14651858.CD006187.pub3
Lees KR, Emberson J, Blackwell L, Bluhmki E, Davis SM, Donnan GA et al (2016) Effects of alteplase for acute stroke on the distribution of functional outcomes: a pooled analysis of 9 trials. Stroke 47(9):2373–2379. https://doi.org/10.1161/STROKEAHA.116.013644
Li Z et al (2018) Effects of early mobilization after acute stroke: a meta-analysis of randomized control trials. J Stroke Cerebrovasc Dis 27(5):1326–1337. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.12.021
Lindley RI, Anderson CS, Billot L, Forster A, Hackett ML, Harvey LA et al (2017) Family-led rehabilitation after stroke in India (ATTEND): a randomised controlled trial. Lancet 390(10094):588–599. https://doi.org/10.1016/S0140-6736(17)31447-2
Marler JR et al (2000) Early stroke treatment associated with better outcome: the NINDS rt-PA Stroke Study. Neurology 55(11):1649–1655. https://doi.org/10.1212/WNL.55.11.1649
Mattioli F et al (2014) Early aphasia rehabilitation is associated with functional reactivation of the left inferior frontal gyrus a pilot study. Stroke 45(2):545–552
Mayo NE (2016) Stroke rehabilitation at home: lessons learned and ways forward. Stroke 47(6):1685–1691. https://doi.org/10.1161/STROKEAHA.116.011309
Meyer S, Verheyden G, Brinkmann N, Dejaeger E, De Weerdt W, Feys H et al (2015) Functional and motor outcome 5 years after stroke is equivalent to outcome at 2 months: follow-up of the collaborative evaluation of rehabilitation in stroke across Europe. Stroke 46(6):1613–1619. https://doi.org/10.1161/STROKEAHA.115.009421
Momosaki R et al (2016) Very early versus delayed rehabilitation for acute ischemic stroke patients with intravenous recombinant tissue plasminogen activator: a nationwide retrospective cohort study. Cerebrovasc Dis 42(1–2):41–48. https://doi.org/10.1159/000444720
National Institute for Health and Care Excellence (NICE) (2013) Stroke rehabilitation in adults. NICE clinical guidelines
NICE (2013) Stroke rehabilitation in adults. Guidance and guidelines, clinical guideline CG162
Nouwens F, Dippel DWJ et al (2013) Rotterdam Aphasia Therapy Study (RATS)-3: “The efficacy of intensive cognitive-linguistic therapy in the acute stage of aphasia”; design of a randomised controlled trial. Trials 14:24. https://doi.org/10.1186/1745-6215-14-24
Ojo O, Brooke J (2016) The use of enteral nutrition in the management of stroke. Nutrients 8(12):827. https://doi.org/10.3390/nu8120827
Owens DK et al (2010) AHRQ Series Paper 5: grading the strength of a body of evidence when comparing medical interventions-Agency for Healthcare Research and Quality and the Effective Health-Care Program. J Clin Epidemiol 63(5):513–523. https://doi.org/10.1016/j.jclinepi.2009.03.009
Palli C et al (2017) Early dysphagia screening by trained nurses reduces pneumonia rate in stroke patients: a clinical intervention study. Stroke 48(9):2583–2585. https://doi.org/10.1161/STROKEAHA.117.018157
Pandian JD, Arora R, Kaur P, Sharma D, Vishwambaran DK, Arima H (2014) Mirror therapy in unilateral neglect after stroke (MUST trial): a randomized controlled trial. Neurology 83(11):1012–1017. https://doi.org/10.1212/WNL.0000000000000773
Pandian JD, Felix C, Kaur P, Sharma D, Julia L, Toor G et al (2015) FAmily-led RehabiliTaTion aftEr stroke in INDia: the ATTEND pilot study. Int J Stroke 10(4):609–614. https://doi.org/10.1111/ijs.12475
Platz T (2019) Evidence-based guidelines and clinical pathways in stroke rehabilitation: an international perspective. Front Neurol 10:200. https://doi.org/10.3389/fneur.2019.00200
Powers WJ et al (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49(3):e46–e110. https://doi.org/10.1161/STR.0000000000000158
Rha JH, Saver JL (2007) The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38(3):967–973. https://doi.org/10.1161/01.STR.0000258112.14918.24
Rice D, Janzen S, McIntyre A, Vermeer J, Britt E, Teasell R (2016) Comprehensive outpatient rehabilitation program: hospital-based stroke outpatient rehabilitation. J Stroke Cerebrovasc Dis 25(5):1158–1164. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.02.007
Rønning OM, Guldvog B (1998) Outcome of subacute stroke rehabilitation: a randomized controlled trial. Stroke 29(4):779–784. https://doi.org/10.1161/01.STR.29.4.779
Ru X, Dai H, Jiang B, Li N, Zhao X, Hong Z et al (2017) Community-based rehabilitation to improve stroke survivors’ rehabilitation participation and functional recovery. Am J Phys Med Rehabil 96(7):e123–e129. https://doi.org/10.1097/PHM.0000000000000650
Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B (2018) Tele-rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis 27(9):2306–2318. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.05.013
Sarı A (2017) Anxiety, Depression And Burnout Levels In Caregivers Of Stroke Patients In A Rehabilitation Hospital. Southern Clinics of Istanbul Eurasia. https://doi.org/10.14744/scie.2017.75046
Schwamm LH et al (2005) Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Circulation 111:1078–1091. https://doi.org/10.1161/01.CIR.0000154252.62394.1E
Scottish Intercollegiate Guidelines Network (2010) Management of patients with stroke: identification and management of dysphagia (SIGN guideline no 119). Scottish Intercollegiate Guidelines Network
Seminog OO et al (2019) Determinants of the decline in mortality from acute stroke in England: linked national database study of 795 869 adults. BMJ (Online) 365:l1778. https://doi.org/10.1136/bmj.l1778
Singh MB (2013) Neurologic disability: a hidden epidemic for India. Neurology 79(21):2146–2147
Smith EE et al (2018) Effect of dysphagia screening strategies on clinical outcomes after stroke: a systematic review for the 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke 49(3):e123–e128. https://doi.org/10.1161/STR.0000000000000159
Stephenson S, Wiles R (2000) Advantages and disadvantages of the home setting for therapy: views of patients and therapists. Br J Occup Ther 63(2):59–64. https://doi.org/10.1177/030802260006300203
Surya N (2010) Neurorehabilitation in India. Neurorehabilitation News Spring; ASNR, p 3
Surya N (2015) Rehabilitation of multiple sclerosis patients in India. Ann Indian Acad Neurol 18(Suppl 1):S43–S47
Teasell R, Foley N, Hussein N, Speechley M (2018) The elements of stroke rehabilitation, evidence-based review of stroke rehabilitation
Van De Port IGL, Kwakkel G, Van Wijk I, Lindeman E (2006) Susceptibility to deterioration of mobility long-term after stroke: a prospective cohort study. Stroke 37(1):167–171. https://doi.org/10.1161/01.STR.0000195180.69904.f2
Vloothuis JDM, Mulder M, Veerbeek JM et al (2016) Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev 12:CD011058
WFNR (2015) Neurorehabilitation in developing countries time for action. http://wfnr.co.uk/education-and-research/position-statements/
WHO (2014) Neurological disorders associated with malnutrition. In: Neurological disorders: public health challenges. WHO, Geneva. https://doi.org/10.1037/e521482010-002
Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC et al (2016) Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 47(6):e98–e169. https://doi.org/10.1161/STR.0000000000000098
Wolfe CDA, Rudd AG (2011) Improvement of care in acute stroke units. Lancet 378:1679–1680. https://doi.org/10.1016/S0140-6736(11)61545-6
Xu T et al (2017) Efficacy and safety of very early mobilization in patients with acute stroke: a systematic review and meta-analysis. Sci Rep 7:6550. https://doi.org/10.1038/s41598-017-06871-z
Yagi M et al (2017) Impact of rehabilitation on outcomes in patients with ischemic stroke: a nationwide retrospective cohort study in Japan. Stroke 48(3):740–746. https://doi.org/10.1161/STROKEAHA.116.015147
Yamada SM (2015) Too early initiation of enteral nutrition is not nutritionally advantageous for comatose acute stroke patients. J Nippon Med Sch 82(4):186–192. https://doi.org/10.1272/jnms.82.186
Zhou X, Du M, Zhou L (2018) Use of mobile applications in post-stroke rehabilitation: a systematic review. Top Stroke Rehabil:1–11. https://doi.org/10.1080/10749357.2018.1482446
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this chapter or parts of it.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this chapter
Cite this chapter
Wasti, S.A., Surya, N., Stephan, K.M., Owolabi, M. (2021). Healthcare Settings for Rehabilitation After Stroke. In: Platz, T. (eds) Clinical Pathways in Stroke Rehabilitation. Springer, Cham. https://doi.org/10.1007/978-3-030-58505-1_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-58505-1_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-58504-4
Online ISBN: 978-3-030-58505-1
eBook Packages: MedicineMedicine (R0)