Abstract
Background
Major depressive disorder (MDD) has detrimental effects on an individual’s personal life, leads to increased risk of comorbidities, and places an enormous economic burden on society. Several ‘second-generation’ antidepressants are available as both immediate-release (IR) and extended-release formulations. The advantage of extended-release formulations may be the potentially improved adherence and a lower risk of adverse events.
Objective
We conducted a systematic review to assess the comparative efficacy, risk of harms, and patients’ adherence of IR and extended-release antidepressants for the treatment of MDD.
Data Source
English-language abstracts were retrieved from PubMed, EMBASE, the Cochrane Library, PsycINFO, and International Pharmaceutical Abstracts from 1980 to October 2012, as well as from reference lists of pertinent review articles and grey literature searches.
Eligibility Criteria
We included head-to-head randomized controlled trials (RCTs) of at least 6 weeks’ duration that compared an IR formulation with an extended-release formulation of the same antidepressant in adult patients with MDD. We also included placebo-controlled trials to conduct a network meta-analysis. To assess harms and adherence, in addition to RCTs, we searched for observational studies with ≥1,000 participants and a follow-up of ≥12 weeks.
Study Appraisal and Synthesis Methods
We dually reviewed abstracts and full texts and assessed quality ratings. Lacking head-to-head evidence for many comparisons of interest, we conducted network meta-analyses using Bayesian methods. Our outcome measure of choice was response on the Hamilton Depression Rating Scale.
Results
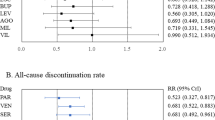
We located seven head-to-head trials and 94 placebo- and active-controlled trials for network meta-analysis. Overall, our analyses indicate that IR and extended-release formulations do not differ substantially with respect to efficacy and risk of harms. The evidence is mixed with respect to differences in adherence, indicating lower adherence for IR formulations.
Limitations
The lack of head-to-head comparisons for many drugs compromises our conclusions. Network meta-analyses have methodological limitations that need to be taken into consideration when interpreting findings.
Conclusion
Available evidence currently shows no clear differences between the two formulations and therefore we cannot recommend a first choice. However, if adherence or compliance with one medication is an issue, then clinicians and patients should consider the alternative medication. If adherence or costs are a problem with one formulation, consideration of the other formulation to provide an adequate treatment trial is reasonable.



Similar content being viewed by others
References
Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602.
Wittchen HU, Jacobi F. Size and burden of mental disorders in Europe: a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol. 2005;15(4):357–76.
Wu E, et al. Comparison of treatment persistence, hospital utilization and costs among major depressive disorder geriatric patients treated with escitalopram versus other SSRI/SNRI antidepressants. Curr Med Res Opin. 2008;24(10):2805–13.
Birnbaum HG, Ben-Hamadi R, Greenberg PE, Hsieh M, Tang J, Reygrobellet C. Determinants of direct cost differences among US employees with major depressive disorders using antidepressants. Pharmacoeconomics. 2009;27:507–17.
Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–56.
DeVane CL. Immediate-release versus controlled-release formulations: pharmacokinetics of newer antidepressants in relation to nausea. J Clin Psychiatry. 2003;64(Suppl 18):14–9.
Kondo T, et al. Altered pharmacokinetics and metabolism of valproate after replacement of conventional valproate with the slow-release formulation in epileptic patients. Pharmacol Toxicol. 2002;90(3):135–8.
Kennedy SH, et al. Combining bupropion SR with venlafaxine, paroxetine, or fluoxetine: a preliminary report on pharmacokinetic, therapeutic, and sexual dysfunction effects. J Clin Psychiatry. 2002;63(3):181–6.
Gartlehner G, et al. Comparative benefits and harms of second-generation antidepressants for treating major depressive disorder: an updated meta-analysis. Ann Intern Med. 2011;155(11):772–85.
Sussman N. Venlafaxine XR therapy for major depression and anxiety disorders: the clinical implications that its advantages pose. Postgrad Med. 1999;106(6 Suppl):31–6.
Keene MS, et al. Adherence to paroxetine CR compared with paroxetine IR in a Medicare-eligible population with anxiety disorders. Am J Manag Care. 2005;11(12 Suppl):S362–9.
Huskamp HA. Prices, profits, and innovation: examining criticisms of new psychotropic drugs’ value. Health Aff (Millwood). 2006;25(3):635–46.
Gartlehner G, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review. Report no. 12-EHC012-EF. Rockville: Agency for Healthcare Research and Quality; Dec 2011.
Chapman A, Morgan LC, Gartlehner G. Semi-automating the manual literature search for systematic reviews increases efficiency. Health Inf Libr J. 2009;27(1):22–7.
Higgins JPT, Altman DG, Sterne J. Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011.
Deeks JJ, et al. Evaluating non-randomised intervention studies. Health Technol Assess, 2003;7(27):iii–x, 1–173.
Jansen JP, et al. Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health. 2008;11(5):956–64.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105–24.
Dias S, et al. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Mak. 2013;33(5):607–17.
Schmidt ME, et al. The efficacy and safety of a new enteric-coated formulation of fluoxetine given once weekly during the continuation treatment of major depressive disorder. J Clin Psychiatry. 2000;61(11):851–7.
Claxton A, et al. Patient compliance to a new enteric-coated weekly formulation of fluoxetine during continuation treatment of major depressive disorder. J Clin Psychiatry. 2000;61(12):928–32.
Rapaport MH, et al. Efficacy of controlled-release paroxetine in the treatment of late-life depression. J Clin Psychiatry. 2003;64(9):1065–74.
Higuchi T, et al. Paroxetine controlled-release formulation in the treatment of major depressive disorder: a randomized, double-blind, placebo-controlled study in Japan and Korea. Psychiatry Clin Neurosci. 2011;65(7):655–63.
Golden RN, et al. Efficacy and tolerability of controlled-release and immediate-release paroxetine in the treatment of depression. J Clin Psychiatry. 2002;63(7):577–84.
Cunningham LA. Once-daily venlafaxine extended release (XR) and venlafaxine immediate release (IR) in outpatients with major depression. Venlafaxine XR 208 Study Group. Ann Clin Psychiatry. 1997;9(3):157–64.
Burke WJ, McArthur-Miller DA. Exploring treatment alternatives: weekly dosing of fluoxetine for the continuation phase of major depressive disorder. J Clin Psychiatry. 2001;62(Suppl 22):38–42.
Feiger A, et al. Nefazodone versus sertraline in outpatients with major depression: focus on efficacy, tolerability, and effects on sexual function and satisfaction. J Clin Psychiatry. 1996;57(Suppl 2):53–62.
Feiger AD, et al. A placebo-controlled study evaluating the efficacy and safety of flexible-dose desvenlafaxine treatment in outpatients with major depressive disorder. CNS Spectr. 2009;14(1):41–50.
Boyer P, et al. Efficacy, safety, and tolerability of fixed-dose desvenlafaxine 50 and 100 mg/day for major depressive disorder in a placebo-controlled trial. Int Clin Psychopharmacol. 2008;23(5):243–53.
Liebowitz MR, Yeung PP, Entsuah R. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in adult outpatients with major depressive disorder. J Clin Psychiatry. 2007;68(11):1663–72.
Septien-Velez L, et al. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in the treatment of major depressive disorder. Int Clin Psychopharmacol. 2007;22(6):338–47.
Brannan SK, et al. Duloxetine 60 mg once-daily in the treatment of painful physical symptoms in patients with major depressive disorder. J Psychiatr Res. 2005;39(1):43–53.
Detke MJ, et al. Duloxetine 60 mg once daily dosing versus placebo in the acute treatment of major depression. J Psychiatr Res. 2002;36(6):383–90.
Detke MJ, et al. Duloxetine, 60 mg once daily, for major depressive disorder: a randomized double-blind placebo-controlled trial. J Clin Psychiatry. 2002;63(4):308–15.
Detke MJ, et al. Duloxetine in the acute and long-term treatment of major depressive disorder: a placebo- and paroxetine-controlled trial. Eur Neuropsychopharmacol. 2004;14(6):457–70.
Wernicke JF, et al. Low-dose fluoxetine therapy for depression. Psychopharmacol Bull. 1988;24(1):183–8.
Lydiard RB, et al. Fluvoxamine, imipramine, and placebo in the treatment of depressed outpatients: effects on depression. Psychopharmacol Bull. 1989;25(1):68–70.
Cohn CK, et al. Responders to antidepressant drug treatment: a study comparing nefazodone, imipramine, and placebo in patients with major depression. J Clin Psychiatry. 1996;57(Suppl 2):15–8.
Fontaine R, et al. A double-blind comparison of nefazodone, imipramine, and placebo in major depression. J Clin Psychiatry. 1994;55(6):234–41.
Rickels K, et al. A placebo-controlled, double-blind, clinical trial of paroxetine in depressed outpatients. Acta Psychiatr Scand Suppl. 1989;350:117–23.
Reimherr FW, et al. Antidepressant efficacy of sertraline: a double-blind, placebo- and amitriptyline-controlled, multicenter comparison study in outpatients with major depression. J Clin Psychiatry. 1990;51(Suppl B):18–27.
Lydiard RB, et al. A double-blind, placebo-controlled study comparing the effects of sertraline versus amitriptyline in the treatment of major depression. J Clin Psychiatry. 1997;58(11):484–91.
Hypericum Depression Trial Study Group. Effect of hypericum perforatum (St John’s wort) in major depressive disorder: a randomized controlled trial. JAMA. 2002;287(14):1807–14.
Olie J, Gunn K, Katz E. A double-blind placebo-controlled multicentre study of sertraline in the acute and continuation treatment of major depression. Eur Psychiatry. 1997;12(1):34–41.
Blumenthal JA, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587–96.
Thase ME. Efficacy and tolerability of once-daily venlafaxine extended release (XR) in outpatients with major depression. The Venlafaxine XR 209 Study Group. J Clin Psychiatry. 1997;58(9):393–8.
Wade A, Gembert K, Florea I. A comparative study of the efficacy of acute and continuation treatment with escitalopram versus duloxetine in patients with major depressive disorder. Curr Med Res Opin. 2007;23(7):1605–14.
Khan A, et al. Double-blind comparison of escitalopram and duloxetine in the acute treatment of major depressive disorder. Clin Drug Investig. 2007;27(7):481–92.
Lee P, et al. Once-daily duloxetine 60 mg in the treatment of major depressive disorder: multicenter, double-blind, randomized, paroxetine-controlled, non-inferiority trial in China, Korea, Taiwan and Brazil. Psychiatry Clin Neurosci. 2007;61(3):295–307.
Feighner JP, et al. Double-blind comparison of bupropion and fluoxetine in depressed outpatients. J Clin Psychiatry. 1991;52(8):329–35.
Mao PX, et al. Escitalopram in major depressive disorder: a multicenter, randomized, double-blind, fixed-dose, parallel trial in a Chinese population. Depress Anxiety. 2008;25(1):46–54.
Hong CJ, et al. A double-blind, randomized, group-comparative study of the tolerability and efficacy of 6 weeks’ treatment with mirtazapine or fluoxetine in depressed Chinese patients. J Clin Psychiatry. 2003;64(8):921–6.
Rush AJ, et al. Comparative effects of nefazodone and fluoxetine on sleep in outpatients with major depressive disorder. Biol Psychiatry. 1998;44(1):3–14.
Gagiano C. A double blind comparison of paroxetine and fluoxetine in patients with major depression. Br J Clin Res. 1993;4:145–52.
De Wilde J, et al. A double-blind, comparative, multicentre study comparing paroxetine with fluoxetine in depressed patients. Acta Psychiatr Scand. 1993;87(2):141–5.
Chouinard G, et al. A Canadian multicenter, double-blind study of paroxetine and fluoxetine in major depressive disorder. J Affect Disord. 1999;54(1–2):39–48.
Sechter D, et al. A double-blind comparison of sertraline and fluoxetine in the treatment of major depressive episode in outpatients. Eur Psychiatry. 1999;14(1):41–8.
Bennie EH, Mullin JM, Martindale JJ. A double-blind multicenter trial comparing sertraline and fluoxetine in outpatients with major depression. J Clin Psychiatry. 1995;56(6):229–37.
Dierick M, et al. A double-blind comparison of venlafaxine and fluoxetine for treatment of major depression in outpatients. Prog Neuropsychopharmacol Biol Psychiatry. 1996;20(1):57–71.
Costa e Silva J. Randomized, double-blind comparison of venlafaxine and fluoxetine in outpatients with major depression. J Clin Psychiatry. 1998;59(7):352–7.
Alves C, Cachola I, Brandao J. Efficacy and tolerability of venlafaxine and fluoxetine in outpatients with major depression. Prim Care Psychiatry. 1999;5(2):52–63.
Tzanakaki M, et al. Increased remission rates with venlafaxine compared with fluoxetine in hospitalized patients with major depression and melancholia. Int Clin Psychopharmacol. 2000;15(1):29–34.
De Nayer A, et al. Venlafaxine compared with fluoxetine in outpatients with depression and concomitant anxiety. Int J Neuropsychopharmacol. 2002;5(2):115–20.
Tylee A, et al. A double-blind, randomized, 12-week comparison study of the safety and efficacy of venlafaxine and fluoxetine in moderate to severe major depression in general practice. Prim Care Psychiatry. 1997;3(1):51–8.
Haffmans PM, Timmerman L, Hoogduin CA. Efficacy and tolerability of citalopram in comparison with fluvoxamine in depressed outpatients: a double-blind, multicentre study. The LUCIFER Group. Int Clin Psychopharmacol. 1996;11(3):157–64.
Hicks JA, et al. Randomised controlled study of sleep after nefazodone or paroxetine treatment in out-patients with depression. Br J Psychiatry. 2002;180:528–35.
Benkert O, Szegedi A, Kohnen R. Mirtazapine compared with paroxetine in major depression. J Clin Psychiatry. 2000;61(9):656–63.
Rush AJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131–8.
Munizza C, et al. A comparative, randomized, double-blind study of trazodone prolonged-release and sertraline in the treatment of major depressive disorder. Curr Med Res Opin. 2006;22(9):1703–13.
Weisler RH, et al. Comparison of bupropion and trazodone for the treatment of major depression. J Clin Psychopharmacol. 1994;14(3):170–9.
van Moffaert M, et al. Mirtazapine is more effective than trazodone: a double-blind controlled study in hospitalized patients with major depression. Int Clin Psychopharmacol. 1995;10(1):3–9.
Kasper S, et al. A comparative, randomised, double-blind study of trazodone prolonged-release and paroxetine in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2005;21(8):1139–46.
Bielski RJ, Ventura D, Chang CC. A double-blind comparison of escitalopram and venlafaxine extended release in the treatment of major depressive disorder. J Clin Psychiatry. 2004;65(9):1190–6.
Sir A, et al. Randomized trial of sertraline versus venlafaxine XR in major depression: efficacy and discontinuation symptoms. J Clin Psychiatry. 2005;66(10):1312–20.
Shelton RC, et al. A randomized, double-blind, active-control study of sertraline versus venlafaxine XR in major depressive disorder. J Clin Psychiatry. 2006;67(11):1674–81.
Boulenger JP, et al. A comparative study of the efficacy of long-term treatment with escitalopram and paroxetine in severely depressed patients. Curr Med Res Opin. 2006;22(7):1331–41.
Ventura D, et al. Escitalopram versus sertraline in the treatment of major depressive disorder: a randomized clinical trial. Curr Med Res Opin. 2007;23(2):245–50.
Perahia DG, et al. Duloxetine in the treatment of major depressive disorder: a placebo- and paroxetine-controlled trial. Eur Psychiatry. 2006;21(6):367–78.
Tourian KA, et al. Desvenlafaxine 50 and 100 mg/d in the treatment of major depressive disorder: an 8-week, phase III, multicenter, randomized, double-blind, placebo-controlled, parallel-group trial and a post hoc pooled analysis of three studies. Clin Ther. 2009;31:1405–23.
Nierenberg AA, et al. Duloxetine versus escitalopram and placebo in the treatment of patients with major depressive disorder: onset of antidepressant action, a non-inferiority study. Curr Med Res Opin. 2007;23(2):401–16.
Goldstein DJ, et al. Duloxetine in the treatment of major depressive disorder: a double-blind clinical trial. J Clin Psychiatry. 2002;63(3):225–31.
Coleman CC, et al. Sexual dysfunction associated with the treatment of depression: a placebo-controlled comparison of bupropion sustained release and sertraline treatment. Ann Clin Psychiatry. 1999;11(4):205–15.
Croft H, et al. A placebo-controlled comparison of the antidepressant efficacy and effects on sexual functioning of sustained-release bupropion and sertraline. Clin Ther. 1999;21(4):643–58.
Coleman CC, et al. A placebo-controlled comparison of the effects on sexual functioning of bupropion sustained release and fluoxetine. Clin Ther. 2001;23(7):1040–58.
Fava M, et al. A double-blind study of paroxetine, fluoxetine, and placebo in outpatients with major depression. Ann Clin Psychiatry. 1998;10(4):145–50.
Rudolph RL, Feiger AD. A double-blind, randomized, placebo-controlled trial of once-daily venlafaxine extended release (XR) and fluoxetine for the treatment of depression. J Affect Disord. 1999;56(2–3):171–81.
Nemeroff CB, Thase ME. A double-blind, placebo-controlled comparison of venlafaxine and fluoxetine treatment in depressed outpatients. J Psychiatric Res. 2007;41(3):351–9.
Fava M, et al. Acute efficacy of fluoxetine versus sertraline and paroxetine in major depressive disorder including effects of baseline insomnia. J Clin Psychopharmacol. 2002;22(2):137–47.
Ou JJ, et al. Efficacy and safety of escitalopram versus citalopram in major depressive disorder: a 6-week, multicenter, randomized, double-blind, flexible-dose study. Psychopharmacology. 2011;213(2–3):639–46.
Barber JP, et al. Short-term dynamic psychotherapy versus pharmacotherapy for major depressive disorder: a randomized, placebo-controlled trial. J Clin Psychiatry. 2012;73(1):66–73.
Dunlop BW, et al. Symptomatic and functional improvement in employed depressed patients: a double-blind clinical trial of desvenlafaxine versus placebo. J Clin Psychopharmacol. 2011;31(5):569–76.
Alvarez E, et al. A double-blind, randomized, placebo-controlled, active reference study of Lu AA21004 in patients with major depressive disorder. Int J Neuropsychopharmacol. 2012;15(5):589–600.
Oakes TM, et al. Assessment of depressive symptoms and functional outcomes in patients with major depressive disorder treated with duloxetine versus placebo: primary outcomes from two trials conducted under the same protocol. Hum Psychopharmacol. 2012;27(1):47–56.
Mehtonen OP, et al. Randomized, double-blind comparison of venlafaxine and sertraline in outpatients with major depressive disorder. Venlafaxine 631 Study Group. J Clin Psychiatry. 2000;61(2):95–100.
Fabre LF, Putman HP 3rd. A fixed-dose clinical trial of fluoxetine in outpatients with major depression. J Clin Psychiatry. 1987;48(10):406–8.
Elliott AJ, et al. Randomized, placebo-controlled trial of paroxetine versus imipramine in depressed HIV-positive outpatients. Am J Psychiatry. 1998;155(3):367–72.
Fabre L, et al. Fluvoxamine versus imipramine and placebo: a double-blind comparison in depressed patients. Int Clin Psychopharmacol. 1996;11(2):119–27.
Feighner JP, Boyer WF. Paroxetine in the treatment of depression: a comparison with imipramine and placebo. J Clin Psychiatry. 1992;53(Suppl):44–7.
Feighner J, et al. A double-blind, placebo-controlled trial of nefazodone in the treatment of patients hospitalized for major depression. J Clin Psychiatry. 1998;59(5):246–53.
Smith WT, Glaudin V. A placebo-controlled trial of paroxetine in the treatment of major depression. J Clin Psychiatry. 1992;53(Suppl):36–9.
Muijen M, et al. A comparative clinical trial of fluoxetine, mianserin and placebo in depressed outpatients. Acta Psychiatr Scand. 1988;78(3):384–90.
Smith WT, et al. Mirtazapine vs. amitriptyline vs. placebo in the treatment of major depressive disorder. Psychopharmacol Bull. 1990;26(2):191–6.
Wernicke J, et al. Fixed-dose fluoxetine therapy for depression. Psychopharmacol Bull. 1987;23(1):164.
Rudolph RL, et al. A randomized, placebo-controlled, dose-response trial of venlafaxine hydrochloride in the treatment of major depression. J Clin Psychiatry. 1998;59(3):116–22.
Rickels K, et al. The efficacy and safety of paroxetine compared with placebo in outpatients with major depression. J Clin Psychiatry. 1992;53(Suppl):30–2.
Rickels K, et al. Nefazodone and imipramine in major depression: a placebo-controlled trial. Br J Psychiatry. 1994;164(6):802–5.
Roy-Byrne PP, et al. Nefazodone treatment of major depression in alcohol-dependent patients: a double-blind, placebo-controlled trial. J Clin Psychopharmacol. 2000;20(2):129–36.
McGrath PJ, et al. A placebo-controlled study of fluoxetine versus imipramine in the acute treatment of atypical depression. Am J Psychiatry. 2000;157(3):344–50.
Hegerl U, et al. Effects of pharmacotherapy and psychotherapy in depressed primary-care patients: a randomized, controlled trial including a patients’ choice arm. Int J Neuropsychopharmacol. 2010;13(1):31–44.
Soares CN, et al. Desvenlafaxine and escitalopram for the treatment of postmenopausal women with major depressive disorder. Menopause. 2010;17(4):700–11.
Beasley CM Jr, et al. Fluoxetine versus trazodone: efficacy and activating-sedating effects. J Clin Psychiatry. 1991;52(7):294–9.
Silverstone PH, Ravindran A. Once-daily venlafaxine extended release (XR) compared with fluoxetine in outpatients with depression and anxiety. Venlafaxine XR 360 Study Group. J Clin Psychiatry. 1999;60(1):22–8.
Lapierre YD, et al. Treatment of major affective disorder with fluvoxamine. J Clin Psychiatry. 1987;48(2):65–8.
Gastpar M, Singer A, Zeller K. Comparative efficacy and safety of a once-daily dosage of hypericum extract STW3-VI and citalopram in patients with moderate depression: a double-blind, randomised, multicentre, placebo-controlled study. Pharmacopsychiatry. 2006;39:66–75.
Goldstein DJ, et al. Duloxetine in the treatment of depression: a double-blind placebo-controlled comparison with paroxetine. J Clin Psychopharmacol. 2004;24(4):389–99.
Claghorn JL. The safety and efficacy of paroxetine compared with placebo in a double-blind trial of depressed outpatients. J Clin Psychiatry. 1992;53(Suppl):33–5.
Corrigan MH, et al. Comparison of pramipexole, fluoxetine, and placebo in patients with major depression. Depress Anxiety. 2000;11(2):58–65.
Clerc GE, Ruimy P, Verdeau-Palles J. A double-blind comparison of venlafaxine and fluoxetine in patients hospitalized for major depression and melancholia. The Venlafaxine French Inpatient Study Group. Int Clin Psychopharmacol. 1994;9(3):139–43.
Gulseren L, et al. Comparison of fluoxetine and paroxetine in type II diabetes mellitus patients. Arch Med Res. 2005;36(2):159–65.
Wade A, et al. A randomized, double-blind, 24-week study comparing the efficacy and tolerability of mirtazapine and paroxetine in depressed patients in primary care. Int Clin Psychopharmacol. 2003;18(3):133–41.
Eisen SA, Miller DK, Woodward RS, Spitznagel E, Przybeck TR. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med. 1990;150(9):1881–4.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23(8):1296–310.
Stang P, Young S, Hogue S. Better patient persistence with once-daily bupropion compared with twice-daily bupropion. Am J Ther. 2007;14(1):20–4.
Consumer Reports Best Buy Drugs™. Using antidepressants to treat depression. 2013. Available from: http://www.consumerreports.org/health/resources/pdf/best-buy-drugs/Antidepressants_update.pdf. Accessed 9 Apr 2014.
Acknowledgments
Network meta-analyses were conducted by Tania Wilkins, PhD (The University of North Carolina at Chapel Hill, Gillings School of Global Public Health Biostatistics, Chapel Hill, NC, USA).
Funding
This project was originally funded under Contract No. HHSA-290-2007-10056I from the AHRQ, US Department of Health and Human Services.
Conflicts of Interest
All authors report grants from the US AHRQ during the conduct of the study.
Barbara Nussbaumer, Laura C. Morgan, Ursula Reichenpfader, Amy Greenblatt, Megan van Noord, Linda Lux, Bradley N. Gaynes, and Gerald Gartlehner declare that they have no conflicts of interest.
Richard A. Hansen declares that he has received personal consulting fees from Novartis, personal fees from Daiichi Sankyo, and personal fees from Allergan outside the submitted work.
Systematic Review Registration Number
This systematic review was not registered, but all AHRQ protocols are available online on their website.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nussbaumer, B., Morgan, L.C., Reichenpfader, U. et al. Comparative Efficacy and Risk of Harms of Immediate- versus Extended-Release Second-Generation Antidepressants: A Systematic Review with Network Meta-Analysis. CNS Drugs 28, 699–712 (2014). https://doi.org/10.1007/s40263-014-0169-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-014-0169-z