Abstract
Background
Although it has been well established that galectin-4 is selectively expressed by intestinal epithelial cells, the role of galectin-4 in colorectal cancer (CRC) development is, as yet, poorly understood. Here, we aimed to explore the role of galectin-4 in CRC development, both in vitro and in vivo.
Methods
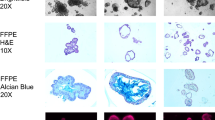
Galectin-4 expression was investigated in tissue specimens from patients with adenoma, carcinoma and ulcerative colitis (UC) using immunohistochemistry. Colorectal cancer-derived HT-29 cells, in which galectin-4 expression was knocked down, were established using shRNA. mRNA and protein expression levels of galectin-4 and several downstream cancer-related genes were analyzed using RT-PCR, qPCR array, Western blotting, and immunofluorescence assays. To investigate the effect of galectin-4 expression abrogation on tumorigenesis in vivo, xenograft assays were performed.
Results
Immunohistochemistry analyses showed high expression levels of galectin-4 in normal colon mucosa tissues. Conversely, the expression levels of galectin-4 were significantly lower in CRC samples and its precursor lesions with dysplasia or inflammation. We found that shRNA-mediated galectin-4 silencing increases cell proliferation and, concomitantly, activates NF-κB and STAT3 signaling along with IL-6 up-regulation. In addition, we found that shRNA-mediated galectin-4 silencing promotes the expression of NF-κB target genes and other cancer-related genes and, concomitantly, enhances the in vivo growth of xenografts.
Conclusions
We show that abrogation of galectin-4 expression promotes cancer cell proliferation and, for the first time, provide evidence that down-regulation of galectin-4 elicits tumor promotion in vitro and in vivo through activation of IL-6/NF-κB/STAT3 signaling.






Similar content being viewed by others
References
F.T. Liu, Galectins: a new family of regulators of inflammation. Clin. Immunol. 97, 79–88 (2000)
N. Rubinstein, J.M. Ilarregui, M.A. Toscano, G.A. Rabinovich, The role of galectins in the initiation, amplification and resolution of the inflammatory response. Tissue Antigens 64, 1–12 (2004)
G.A. Rabinovich, M.A. Toscano, Turning ‘sweet’ on immunity: galectin-glycan interactions in immune tolerance and inflammation. Nat. Rev. Immunol. 9, 338–352 (2009)
M.E. Huflejt, H. Leffler, Galectin-4 in normal tissues and cancer. Glycoconj. J. 20, 247–255 (2004)
D. Paclik, S. Danese, U. Berndt, B. Wiedenmann, A. Dignass, A. Sturm, Galectin-4 controls intestinal inflammation by selective regulation of peripheral and mucosal T cell apoptosis and cell cycle. PLoS One 3, e2629 (2008)
M. van de Wetering, E. Sancho, C. Verweij, W. de Lau, I. Oving, A. Hurlstone, K. van der Horn, E. Batlle, D. Coudreuse, A.P. Haramis, M. Tjon-Pon-Fong, P. Moerer, M. van den Born, G. Soete, S. Pals, M. Eilers, R. Medema, H. Clevers, The beta-catenin/TCF-4 complex imposes a crypt progenitor phenotype on colorectal cancer cells. Cell 111, 241–250 (2002)
M.A. Wooters, M.B. Hildreth, E.A. Nelson, A.K. Erickson, Immunohistochemical characterization of the distribution of galectin-4 in porcine small intestine. J. Histochem. Cytochem. 53, 197–205 (2005)
K. Kim, U. Park, J. Wang, J. Lee, S. Park, S. Kim, D. Choi, C. Kim, J. Park, Gene profiling of colonic serrated adenomas by using oligonucleotide microarray. Int. J. Colorectal Dis. 23, 569–580 (2008)
A. Satelli, P.S. Rao, S. Thirumala, U.S. Rao, Galectin-4 functions as a tumor suppressor of human colorectal cancer. Int. J. Cancer 129, 799–809 (2011)
H. Barrow, X. Guo, H.H. Wandall, J.W. Pedersen, B. Fu, Q. Zhao, C. Chen, J.M. Rhodes, L.G. Yu, Serum galectin-2, -4, and -8 are greatly increased in colon and breast cancer patients and promote cancer cell adhesion to blood vascular endothelium. Clin. Cancer Res. 17, 7035–7046 (2011)
M. Watanabe, I. Takemasa, N. Kaneko, Y. Yokoyama, E. Matsuo, S. Iwasa, M. Mori, N. Matsuura, M. Monden, O. Nishimura, Clinical significance of circulating galectins as colorectal cancer markers. Oncol. Rep. 25, 1217–1226 (2011)
A. Hokama, E. Mizoguchi, K. Sugimoto, Y. Shimomura, Y. Tanaka, M. Yoshida, S.T. Rietdijk, Y.P. de Jong, S.B. Snapper, C. Terhorst, R.S. Blumberg, A. Mizoguchi, Induced reactivity of intestinal CD4(+) T cells with an epithelial cell lectin, galectin-4, contributes to exacerbation of intestinal inflammation. Immunity 20, 681–693 (2004)
J. Bollrath, F.R. Greten, IKK/NF-kappaB and STAT3 pathways: central signalling hubs in inflammation-mediated tumour promotion and metastasis. EMBO Rep 10, 1314–1319 (2009)
H. Lee, A. Herrmann, J.H. Deng, M. Kujawski, G. Niu, Z. Li, S. Forman, R. Jove, D.M. Pardoll, H. Yu, Persistently activated Stat3 maintains constitutive NF-kappaB activity in tumors. Cancer Cell 15, 283–293 (2009)
D. Iliopoulos, H.A. Hirsch, K. Struhl, An epigenetic switch involving NF-kappaB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell 139, 693–706 (2009)
S.I. Grivennikov, M. Karin, Dangerous liaisons: STAT3 and NF-kappaB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev. 21, 11–19 (2010)
D. Vogiagis, W. Brown, E.M. Glare, P.E. O’Brien, Rat colorectal tumours treated with a range of non-steroidal anti-inflammatory drugs show altered cyclooxygenase-2 and cyclooxygenase-1 splice variant mRNA expression levels. Carcinogenesis 22, 869–874 (2001)
S. Grosch, I. Tegeder, E. Niederberger, L. Brautigam, G. Geisslinger, COX-2 independent induction of cell cycle arrest and apoptosis in colon cancer cells by the selective COX-2 inhibitor celecoxib. FASEB J. 15, 2742–2744 (2001)
J. Renkonen, H. Wolff, T. Paavonen, Expression of cyclo-oxygenase-2 in human tongue carcinoma and its precursor lesions. Virchows Arch 440, 594–597 (2002)
D. Piancatelli, P. Romano, P. Sebastiani, D. Adorno, C.U. Casciani, Local expression of cytokines in human colorectal carcinoma: evidence of specific interleukin-6 gene expression. J. Immunother. 22, 25–32 (1999)
S.H. Song, H.S. Jong, H.H. Choi, H. Inoue, T. Tanabe, N.K. Kim, Y.J. Bang, Transcriptional silencing of Cyclooxygenase-2 by hyper-methylation of the 5′ CpG island in human gastric carcinoma cells. Cancer Res. 61, 4628–4635 (2001)
J.R. Vane, Y.S. Bakhle, R.M. Botting, Cyclooxygenases 1 and 2. Annu. Rev. Pharmacol. Toxicol. 38, 97–120 (1998)
T. Nakajima, S. Kinoshita, T. Sasagawa, K. Sasaki, M. Naruto, T. Kishimoto, S. Akira, Phosphorylation at threonine-235 by a ras-dependent mitogen-activated protein kinase cascade is essential for transcription factor NF-IL6. Proc. Natl. Acad. Sci. U. S. A. 90, 2207–2211 (1993)
S.W. Kim, H.M. Kim, K.M. Yang, S.A. Kim, S.K. Kim, M.J. An, J.J. Park, S.K. Lee, T.I. Kim, W.H. Kim, J.H. Cheon, Bifidobacterium lactis inhibits NF-kappaB in intestinal epithelial cells and prevents acute colitis and colitis-associated colon cancer in mice. Inflamm. Bowel Dis. 16, 1514–1525 (2010)
A.C. Ruifrok, D.A. Johnston, Quantification of histochemical staining by color deconvolution. Anal. Quant. Cytol. Histol. 23, 291–299 (2001)
G. Kruppa, B. Thoma, T. Machleidt, K. Wiegmann, M. Kronke, Inhibition of tumor necrosis factor (TNF)-mediated NF-kappa B activation by selective blockade of the human 55-kDa TNF receptor. J. Immunol. 148, 3152–3157 (1992)
S.O. Lee, Y.J. Jeong, H.G. Im, C.H. Kim, Y.C. Chang, I.S. Lee, Silibinin suppresses PMA-induced MMP-9 expression by blocking the AP-1 activation via MAPK signaling pathways in MCF-7 human breast carcinoma cells. Biochem. Biophys. Res. Commun. 354, 165–171 (2007)
S.A. Lang, C. Moser, A. Gaumann, D. Klein, G. Glockzin, F.C. Popp, M.H. Dahlke, P. Piso, H.J. Schlitt, E.K. Geissler, O. Stoeltzing, Targeting heat shock protein 90 in pancreatic cancer impairs insulin-like growth factor-I receptor signaling, disrupts an interleukin-6/signal-transducer and activator of transcription 3/hypoxia-inducible factor-1alpha autocrine loop, and reduces orthotopic tumor growth. Clin. Cancer Res. 13, 6459–6468 (2007)
S.S. Sikandar, K.T. Pate, S. Anderson, D. Dizon, R.A. Edwards, M.L. Waterman, S.M. Lipkin, NOTCH signaling is required for formation and self-renewal of tumor-initiating cells and for repression of secretory cell differentiation in colon cancer. Cancer Res. 70, 1469–1478 (2010)
Y. Okugawa, C. Miki, Y. Toiyama, H. Yasuda, T. Yokoe, S. Saigusa, J. Hiro, K. Tanaka, Y. Inoue, M. Kusunoki, Loss of tumoral expression of soluble IL-6 receptor is associated with disease progression in colorectal cancer. Br. J. Cancer 103, 787–795 (2010)
R. Goswami, M.H. Kaplan, A brief history of IL-9. J. Immunol. 186, 3283–3288 (2011)
S. Grivennikov, M. Karin, Autocrine IL-6 signaling: a key event in tumorigenesis? Cancer Cell 13, 7–9 (2008)
F.M. Corvinus, C. Orth, R. Moriggl, S.A. Tsareva, S. Wagner, E.B. Pfitzner, D. Baus, R. Kaufmann, L.A. Huber, K. Zatloukal, H. Beug, P. Ohlschlager, A. Schutz, K.J. Halbhuber, K. Friedrich, Persistent STAT3 activation in colon cancer is associated with enhanced cell proliferation and tumor growth. Neoplasia 7, 545–555 (2005)
Y.C. Chung, Y.F. Chang, Serum interleukin-6 levels reflect the disease status of colorectal cancer. J. Surg. Oncol. 83, 222–226 (2003)
P.C. Smith, E.T. Keller, Anti-interleukin-6 monoclonal antibody induces regression of human prostate cancer xenografts in nude mice. Prostate 48, 47–53 (2001)
Y. Li, C. de Haar, M. Chen, J. Deuring, M.M. Gerrits, R. Smits, B. Xia, E.J. Kuipers, C.J. van der Woude, Disease-related expression of the IL6/STAT3/SOCS3 signalling pathway in ulcerative colitis and ulcerative colitis-related carcinogenesis. Gut 59, 227–235 (2010)
Y. Yoshida, A. Kumar, Y. Koyama, H. Peng, A. Arman, J.A. Boch, P.E. Auron, Interleukin 1 activates STAT3/nuclear factor-kappaB cross-talk via a unique TRAF6- and p65-dependent mechanism. J. Biol. Chem. 279, 1768–1776 (2004)
M.W. Mayo, L.V. Madrid, S.D. Westerheide, D.R. Jones, X.J. Yuan, A.S. Baldwin Jr., Y.E. Whang, PTEN blocks tumor necrosis factor-induced NF-kappa B-dependent transcription by inhibiting the transactivation potential of the p65 subunit. J. Biol. Chem. 277, 11116–11125 (2002)
S. Grivennikov, E. Karin, J. Terzic, D. Mucida, G.Y. Yu, S. Vallabhapurapu, J. Scheller, S. Rose-John, H. Cheroutre, L. Eckmann, M. Karin, IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell 15, 103–113 (2009)
S. Yoon, S.U. Woo, J.H. Kang, K. Kim, H.J. Shin, H.S. Gwak, S. Park, Y.J. Chwae, NF-kappaB and STAT3 cooperatively induce IL6 in starved cancer cells, Oncogene. (2011)
S. Legrand-Poels, S. Schoonbroodt, J. Piette, Regulation of interleukin-6 gene expression by pro-inflammatory cytokines in a colon cancer cell line. Biochem. J. 349(Pt 3), 765–773 (2000)
W. Vanden Berghe, L. Vermeulen, G. De Wilde, K. De Bosscher, E. Boone, G. Haegeman, Signal transduction by tumor necrosis factor and gene regulation of the inflammatory cytokine interleukin-6. Biochem. Pharmacol. 60, 1185–1195 (2000)
L.H. Wei, M.L. Kuo, C.A. Chen, C.H. Chou, K.B. Lai, C.N. Lee, C.Y. Hsieh, Interleukin-6 promotes cervical tumor growth by VEGF-dependent angiogenesis via a STAT3 pathway. Oncogene 22, 1517–1527 (2003)
M.J. Murnane, J. Cai, S. Shuja, D. McAneny, J.B. Willett, Active matrix metalloproteinase-2 activity discriminates colonic mucosa, adenomas with and without high-grade dysplasia, and cancers. Hum. Pathol. 42, 688–701 (2011)
S. Ramasamy, S. Duraisamy, S. Barbashov, T. Kawano, S. Kharbanda, D. Kufe, The MUC1 and galectin-3 oncoproteins function in a microRNA-dependent regulatory loop. Mol. Cell 27, 992–1004 (2007)
S.E. Baldus, S.P. Monig, F.G. Hanisch, T.K. Zirbes, U. Flucke, S. Oelert, G. Zilkens, B. Madejczik, J. Thiele, P.M. Schneider, A.H. Holscher, H.P. Dienes, Comparative evaluation of the prognostic value of MUC1, MUC2, sialyl-Lewis(a) and sialyl-Lewis(x) antigens in colorectal adenocarcinoma. Histopathology 40, 440–449 (2002)
E.L. Lagow, D.D. Carson, Synergistic stimulation of MUC1 expression in normal breast epithelia and breast cancer cells by interferon-gamma and tumor necrosis factor-alpha. J. Cell. Biochem. 86, 759–772 (2002)
Y.Y. Li, L.L. Hsieh, R.P. Tang, S.K. Liao, K.Y. Yeh, Interleukin-6 (IL-6) released by macrophages induces IL-6 secretion in the human colon cancer HT-29 cell line. Hum. Immunol. 70, 151–158 (2009)
C.L. Hattrup, S.J. Gendler, MUC1 alters oncogenic events and transcription in human breast cancer cells. Breast Cancer Res 8, R37 (2006)
R. Ahmad, D. Raina, V. Trivedi, J. Ren, H. Rajabi, S. Kharbanda, D. Kufe, MUC1 oncoprotein activates the IkappaB kinase beta complex and constitutive NF-kappaB signalling. Nat. Cell Biol. 9, 1419–1427 (2007)
W.L. Smith, D.L. DeWitt, R.M. Garavito, Cyclooxygenases: structural, cellular, and molecular biology. Annu. Rev. Biochem. 69, 145–182 (2000)
D. Tardieu, J.P. Jaeg, A. Deloly, D.E. Corpet, J. Cadet, C.R. Petit, The COX-2 inhibitor nimesulide suppresses superoxide and 8-hydroxy-deoxyguanosine formation, and stimulates apoptosis in mucosa during early colonic inflammation in rats. Carcinogenesis 21, 973–976 (2000)
J.L. Masferrer, K.M. Leahy, A.T. Koki, B.S. Zweifel, S.L. Settle, B.M. Woerner, D.A. Edwards, A.G. Flickinger, R.J. Moore, K. Seibert, Antiangiogenic and antitumor activities of cyclooxygenase-2 inhibitors. Cancer Res. 60, 1306–1311 (2000)
Acknowledgments
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (grant number 2009-0069149) and a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (grant number A120176). We would like to thank the tissue donors for their contribution to this study.
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.W., Park, K.C., Jeon, S.M. et al. Abrogation of galectin-4 expression promotes tumorigenesis in colorectal cancer. Cell Oncol. 36, 169–178 (2013). https://doi.org/10.1007/s13402-013-0124-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-013-0124-x