Abstract
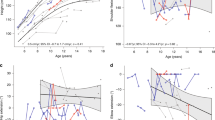
The follow-up of eight Japanese children with Langerhans cell histiocytosis (LCH)-related neurodegenerative central nervous system (ND-CNS) disease who were treated with intravenous immunoglobulin (IVIG) for >3 years is described. The patients developed ND-CNS disease at a median age of 5.2 (range 3.5–10.0) years and received IVIG treatment for a median duration of 6.5 + (range 3.7 to 10+) years. After a median follow-up period of 11.6 + (8.3+ to 13.9+) years after ND-CNS disease diagnosis, the median Expanded Disability Status Scale (EDSS) score of the eight patients was 4.0 (range 2.0–9.5). At the last follow-up as of March 2014, three patients have low EDSS scores (<3.0) and can walk without any assistance. Another three patients have EDSS scores of 3.5–4.5 and can walk by themselves, albeit occasionally with supports. However, the remaining two patients are wheelchair bound or bed ridden. The school performance of seven of the eight patients was below average. IVIG appeared to be most beneficial when it was administered soon after ND-CNS disease diagnosis when the EDSS scores were low (1.0–2.5). The patients who began receiving IVIG when their high EDSS scores were higher (4.5–7.0) appeared to obtain less benefit. To prevent progression of ND-CNS disease in patients with LCH, it is recommended to introduce IVIG early and to continue this therapy for >3 years.
Similar content being viewed by others
References
Badalian-Very G, Vergilio JA, Fleming M, Rollins BJ. Pathogenesis of Langerhans cell histiocytosis. Annu Rev Pathol. 2013;8:1–20.
Grois NG, Favara BE, Mostbeck GH, et al. Central nervous system disease in Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998;12:287–305.
Grois N, Barkovich AJ, Rosenau W, et al. Central nervous system disease associated with Langerhans’ cell histiocytosis. Am J Pediatr Hematol Oncol. 1993;15:245–54.
Prosch H, Grois N, Wnorowski M, Steiner M, Prayer D. Long-term MR imaging course of neurodegenerative Langerhans cell histiocytosis. AJNR Am J Neuroradiol. 2007;28:1022–8.
Martin-Duverneuil N, Idbaih A, Hoang-Xuan K, et al. MRI features of neurodegenerative Langerhans cell histiocytosis. Eur Radiol. 2006;16:2074–82.
Wnorowski M, Prosch H, Prayer D, Janssen G, Gadner H, Grois N. Pattern and course of neurodegeneration in Langerhans cell histiocytosis. J Pediatr. 2008;153:127–32.
Poe LB, Dubowy RL, Hochhauser L, et al. Demyelinating and gliotic cerebellar lesions in Langerhans cell histiocytosis. Am J Neuroradiol. 1994;15:1921–8.
Grois N, Prayer D, Prosch H, et al. CNS LCH Co-operative Group; Neuropathology of CNS disease in Langerhans cell histiocytosis. Brain. 2005;128:829–38.
Imashuku S. High dose immunoglobulin (IVIG) may reduce the incidence of Langerhans cell histiocytosis (LCH)-associated central nervous system involvement. CNS Neurol Disord Drug Targets. 2009;8:380–6.
Imashuku S, Okazaki NA, Nakayama M, et al. Treatment of neurodegenerative CNS disease in Langerhans cell histiocytosis with a combination of intravenous immunoglobulin and chemotherapy. Pediatr Blood Cancer. 2008;50(2):308–11.
Imashuku S, Shioda Y, Kobayashi R, et al. Neurodegenerative central nervous system disease as late sequelae of Langerhans cell histiocytosis. Report from the Japan LCH Study Group. Haematologica. 2008;93(4):615–8.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33:1444–52.
Schmitz-Hübsch T, Tezenas du Montcel S, Baliko L, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66:1717–20.
Allen CE, Flores R, Rauch R, et al. Neurodegenerative central nervous system Langerhans cell histiocytosis and coincident hydrocephalus treated with vincristine/cytosine arabinoside. Pediatr Blood Cancer. 2010;54:416–23.
Kershenovich A, Price AV, Koral K, et al. Failure to treat obstructive hydrocephalus with endoscopic third ventriculostomy in a patient with neurodegenerative Langerhans cell histiocytosis. J Neurosurg Pediatr. 2008;2:304–9.
Barthez MA, Araujo E, Donadieu J. Langerhans cell histiocytosis and the central nervous system in childhood: evolution and prognostic factors. Results of a collaborative study. J Child Neurol. 2000;15:150–6.
Grois N, Posch H, Lassmann H. Prayer, D. In: Weitzman S, Egeler RM, editors. Histiocytic disorders of children and adults. England: Cambridge University Press; 2005. p. 208–28.
Laurencikas E, Gavhed D, Stålemark H, et al. Incidence and pattern of radiological central nervous system Langerhans cell histiocytosis in children: a population based study. Pediatr Blood Cancer. 2011;56:250–7.
Gavhed D, Laurencikas E, Akefeldt SO, Henter JI. Fifteen years of treatment with intravenous immunoglobulin in central nervous system Langerhans cell histiocytosis. Acta Paediatr. 2011;100:e36–9.
Idbaih A, Donadieu J, Barthez MA, et al. Retinoic acid therapy in “degenerative-like” neuro-Langerhans cell histiocytosis: a prospective pilot study. Pediatr Blood Cancer. 2004;43:55–8.
Morimoto Y, Yoshida N, Kawashima N, et al. Identification of predictive factors for response to intravenous immunoglobulin treatment in children with immune thrombocytopenia. Int J Hematol. 2014;99:597–602.
Winkelmann A, Zettl UK. Use of intravenous immunoglobulin in the treatment of immune-mediated demyelinating diseases of the nervous system. Curr Pharm Des. 2012;18:4570–82.
Greenlee JE. Treatment of paraneoplastic cerebellar degeneration. Curr Treat Options Neurol. 2013;15:185–200.
Fahrner B, Prosch H, Minkov M, et al. Long-term outcome of hypothalamic pituitary tumors in Langerhans cell histiocytosis. Pediatr Blood Cancer. 2012;58:606–10.
Acknowledgments
We thank Drs. Hisashi Wakita and Yoko Shioda for providing the update of the 2 patients (Cases 9 and 10) and Yasuko Hashimoto at the JLSG office for her contribution to data collection.
Conflict of interest
The authors declare that there are no conflicts of interests regarding the publication of this paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Imashuku, S., Fujita, N., Shioda, Y. et al. Follow-up of pediatric patients treated by IVIG for Langerhans cell histiocytosis (LCH)-related neurodegenerative CNS disease. Int J Hematol 101, 191–197 (2015). https://doi.org/10.1007/s12185-014-1717-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1717-5