Abstract
Introduction
The aim of this study was to compare survival outcomes in patients enlisted for liver transplantation following liver resection for hepatocellular carcinoma before or at recurrence.
Methods
All patients enlisted for liver transplantation following liver resection for hepatocellular carcinoma from 1996 to 2013 were included and compared according to their status at the time of enlistment: before (de principe) or at (salvage) recurrence. Primary end-point was survival since resection.
Results
One hundred and twenty-one patients were enlisted for liver transplantation following liver resection for hepatocellular carcinoma. Ten patients enlisted for cirrhosis decompensation were excluded from the analysis. Sixty-three patients were enlisted de principe, and 48 for a salvage transplantation. Eleven patients dropped-out. According to per-protocol analysis, the mean diameter of the largest tumor was the only different pathological characteristic of initial resection between groups (31.6 mm in the de principe group versus 48.3 in the salvage, p = 0.017). The 5-year overall survival rate was significantly increased in the de principe group compared to salvage (84.6 versus 74.8 %, p = 0.017). In a multivariate analysis, the salvage strategy was the only independent prognostic factor for death (p = 0.040; OR = 2.5 [1.1–5.8]).
Conclusion
De principe enlistment for liver transplantation following liver resection for hepatocellular carcinoma is associated with greater survival.







Similar content being viewed by others
References
Llovet JM, Burroughs A, and Bruix J. Hepatocellular carcinoma. Lancet 2003;362:1907-1917.
Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, Camerini T, Roayaie S, Schwartz ME, Grazi GL, Adam R, Neuhaus P, Salizzoni M, Bruix J, Forner A, De Carlis L, Cillo U, Burroughs AK, Troisi R, Rossi M, Gerunda GE, Lerut J, Belghiti J, Boin I, Gugenheim J, Rochling F, Van Hoek B, Majno P, and Metroticket Investigator Study G. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 2009;10:35-43.
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, and Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693-699.
Yao FY, Bass NM, Nikolai B, Davern TJ, Kerlan R, Wu V, Ascher NL, and Roberts JP. Liver transplantation for hepatocellular carcinoma: analysis of survival according to the intention-to-treat principle and dropout from the waiting list. Liver Transpl 2002;8:873-883.
Llovet JM, Fuster J, and Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 1999;30:1434-1440.
Llovet JM, Bru C, and Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 1999;19:329-338.
Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A, and Group OLTfHC. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol 2012;13:e11-22.
Proneth A, Zeman F, Schlitt HJ, and Schnitzbauer AA. Is resection or transplantation the ideal treatment in patients with hepatocellular carcinoma in cirrhosis if both are possible? A systematic review and metaanalysis. Ann Surg Oncol 2014;21:3096-3107.
Torzilli G, Belghiti J, Kokudo N, Takayama T, Capussotti L, Nuzzo G, Vauthey JN, Choti MA, De Santibanes E, Donadon M, Morenghi E, and Makuuchi M. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations?: an observational study of the HCC East-West study group. Ann Surg 2013;257:929-937.
Chang CH, Chau GY, Lui WY, Tsay SH, King KL, and Wu CW. Long-term results of hepatic resection for hepatocellular carcinoma originating from the noncirrhotic liver. Arch Surg 2004;139:320-325.
Fuster J, Garcia-Valdecasas JC, Grande L, Tabet J, Bruix J, Anglada T, Taura P, Lacy AM, Gonzalez X, Vilana R, Bru C, Sole M, and Visa J. Hepatocellular carcinoma and cirrhosis. Results of surgical treatment in a European series. Ann Surg 1996;223:297-302.
Majno PE, Sarasin FP, Mentha G, and Hadengue A. Primary liver resection and salvage transplantation or primary liver transplantation in patients with single, small hepatocellular carcinoma and preserved liver function: an outcome-oriented decision analysis. Hepatology 2000;31:899-906.
Cherqui D, Laurent A, Mocellin N, Tayar C, Luciani A, Van Nhieu JT, Decaens T, Hurtova M, Memeo R, Mallat A, and Duvoux C. Liver resection for transplantable hepatocellular carcinoma: long-term survival and role of secondary liver transplantation. Ann Surg 2009;250:738-746.
Adam R, Azoulay D, Castaing D, Eshkenazy R, Pascal G, Hashizume K, Samuel D, and Bismuth H. Liver resection as a bridge to transplantation for hepatocellular carcinoma on cirrhosis: a reasonable strategy? Ann Surg 2003;238:508-518.
Poon RT, Fan ST, Lo CM, Liu CL, and Wong J. Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Ann Surg 2002;235:373-382.
Sala M, Fuster J, Llovet JM, Navasa M, Sole M, Varela M, Pons F, Rimola A, Garcia-Valdecasas JC, Bru C, Bruix J, and Barcelona Clinic Liver Cancer G. High pathological risk of recurrence after surgical resection for hepatocellular carcinoma: an indication for salvage liver transplantation. Liver Transpl 2004;10:1294-1300.
Scatton O, Zalinski S, Terris B, Lefevre JH, Casali A, Massault PP, Conti F, Calmus Y, and Soubrane O. Hepatocellular carcinoma developed on compensated cirrhosis: resection as a selection tool for liver transplantation. Liver Transpl 2008;14:779-788.
Belghiti J, Cortes A, Abdalla EK, Regimbeau JM, Prakash K, Durand F, Sommacale D, Dondero F, Lesurtel M, Sauvanet A, Farges O, and Kianmanesh R. Resection prior to liver transplantation for hepatocellular carcinoma. Ann Surg 2003;238:885-892.
Fuks D, Dokmak S, Paradis V, Diouf M, Durand F, and Belghiti J. Benefit of initial resection of hepatocellular carcinoma followed by transplantation in case of recurrence: an intention-to-treat analysis. Hepatology 2012;55:132-140.
Nathan H, Schulick RD, Choti MA, and Pawlik TM. Predictors of survival after resection of early hepatocellular carcinoma. Ann Surg 2009;249:799-805.
Shah SA, Cleary SP, Wei AC, Yang I, Taylor BR, Hemming AW, Langer B, Grant DR, Greig PD, and Gallinger S. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery 2007;141:330-339.
Cha C, Fong Y, Jarnagin WR, Blumgart LH, and DeMatteo RP. Predictors and patterns of recurrence after resection of hepatocellular carcinoma. J Am Coll Surg 2003;197:753-758.
Jonas S, Bechstein WO, Steinmuller T, Herrmann M, Radke C, Berg T, Settmacher U, and Neuhaus P. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology 2001;33:1080-1086.
Author information
Authors and Affiliations
Corresponding author
Additional information
Primary Discussant
Sean P. Cleary, M.D. (Toronto, ON, Canada)
Thank you for that excellent presentation. You and your colleagues at Beaujon and Pitié Salpêtrière are to be congratulated on this excellent work that provides an insight into this truly unique experience in de principe transplantation at your centers. The concept of de principe transplantation is certainly an attractive one given the mixed outcomes of salvage transplantation and the frequency with which patients develop recurrence outside of transplant criteria following resection.
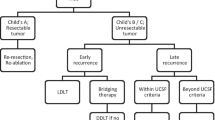
1. In order for us to properly understand this retrospective analysis, I wonder if you could give us some indication as to how patients were for the de principe approach? It would seem from the data that patients in the de principe group had a higher rate of severe fibrosis and non-anatomic resections. Was the decision to list the patient for the de principe approach based on preoperative or postoperative pathologic factors?
2. In your proposed algorithm, you suggest limiting the de principe approach to patients who are within Milan criteria but have negative prognostic factors at the time of resection. Do you feel there is any benefit to de principe transplantation in patients that do not meet that criteria either because of good prognostic features or cancers outside Milan? The latter outside Milan group would be of particular interest given the implications that patients could be downstaged by resection prior to transplantation.
3. Finally, a skeptical view of these results would suggest that the improved outcomes of the de principe group are largely the result of patients who did not have recurrence at the time of transplantation, since the outcome patients who had recurrence in the de principe group appear similar to those treated with salvage transplantation. Furthermore, skeptics might also suggest that patients transplanted de principe without recurrence might not need transplantation. How would you and your group respond to these skeptics?
Closing Discussant
Dr. Tribillon
1. The decision to list the patient for a de principe liver transplantation was based on postoperative pathological factors. This strategy was adopted in both centers following the analysis of their respective series. The prognostic factors that were considered to decide whether the patient would be enlisted de principe or not were as follows: vascular invasion, differentiation, satellite nodules, margins, and underlying cirrhosis. Indeed, this can explain the higher rate of severe fibrosis in the de principe group.
2. It is true that limiting indications for liver transplantation to patients who fulfill Milan criteria is a concern, as these criteria are very restrictive. But, at this time, there is no evidence for us to answer that question. However, our feeling is that regarding patients beyond Milan criteria, primary liver resection, and the use of pathological analysis of the resected specimen, could allow us to identify a sub-group of patients who could benefit from a secondary liver transplantation, as part of a downstaging strategy.
3. I totally understand your point of view. It is not surprising that these patients had better survival outcomes since some of them did not recur at the time of liver transplantation. But, a patient who once had hepatocellular carcinoma, even if it was resected, should not be considered the same as a patient who never had tumoral history. For patients who underwent liver resection for hepatocellular carcinoma, if bad prognostic factors are present at pathological analysis, the recurrence rate can reach 80 %. For these patients, we think it is legitimate to propose liver transplantation before tumor recurrence.
Rights and permissions
About this article
Cite this article
Tribillon, E., Barbier, L., Goumard, C. et al. When Should We Propose Liver Transplant After Resection of Hepatocellular Carcinoma? A Comparison of Salvage and De Principe Strategies. J Gastrointest Surg 20, 66–76 (2016). https://doi.org/10.1007/s11605-015-3018-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-3018-6