Abstract
Background
Dissection requirements differ between various methods for inguinal hernia repair, which may affect operation times, pain response and possibly recovery time. The objectives of this study were to establish if any differences concerning these aspects could be detected following three principally different techniques for primary inguinal hernia repair.
Methods
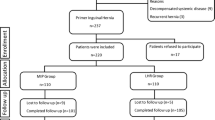
A total of 472 men between 30 and 75 years of age with primary inguinal hernias were included in a prospective controlled study and randomised to Lichtenstein mesh (L), PerFix Plug® (P) or the Prolene® Hernia System (PHS) procedure. All patients were seen and data were collected after 2 weeks, 3 months, 1 year and 3 years.
Results
The follow-up rates were 100, 99.8, 98.7 and 95.3%, respectively. The mean operation time was shorter for P (35.5 min, P < 0.001) and PHS (37.4 min, P < 0.02) versus L (40.4 min). More than 85% of the procedures were performed under local anaesthesia. There were no statistically significant differences between the groups concerning early or late complications, return to full functional ability, early pain response, analgesic consumption or the studied late-outcome parameters after 3 years of observation. Seven (1.5%) evenly distributed recurrences were registered.
Conclusion
All of the techniques are suitable for operation under local anaesthesia. The PHS and P techniques can be performed with shorter operation times than the L method. Early and late outcomes are, however, comparable, with no significant differences concerning complication rates, return to full functional status and/or pain response.





Similar content being viewed by others
References
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83(5):1045–1051, v–vi
Nordin P (2006) Swedish Hernia Register Annual Report. Available online at: http://www.svensktbrackregister.se/pdf/red06.pdf
Kingsnorth AN, Porter CS, Bennett DH, Walker AJ, Hyland ME, Sodergren S (2000) Lichtenstein patch or Perfix plug-and-patch in inguinal hernia: a prospective double-blind randomized controlled trial of short-term outcome. Surgery 127(3):276–283
Kingsnorth AN, Wright D, Porter CS, Robertson G (2002) Prolene Hernia System compared with Lichtenstein patch: a randomised double blind study of short-term and medium-term outcomes in primary inguinal hernia repair. Hernia 6(3):113–119
Bringman S, Ramel S, Heikkinen TJ, Englund T, Westman B, Anderberg B (2003) Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein: a prospective randomized controlled trial. Ann Surg 237(1):142–147
Nienhuijs S, Kortmann B, Boerma M, Strobbe L, Rosman C (2004) Preferred mesh-based inguinal hernia repair in a teaching setting: results of a randomized study. Arch Surg 139(10):1097–1100
Sanjay P, Harris D, Jones P, Woodward A (2006) Randomized controlled trial comparing prolene hernia system and Lichtenstein method for inguinal hernia repair. ANZ J Surg 76(7):548–552
Frey DM, Wildisen A, Hamel CT, Zuber M, Oertli D, Metzger J (2007) Randomized clinical trial of Lichtenstein’s operation versus mesh plug for inguinal hernia repair. Br J Surg 94(1):36–41
Gilbert AI, Graham MF, Voigt WJ (1999) A bilayer patch device for inguinal hernia repair. Hernia 3:161–166
Gilbert AI, Young J, Graham MF, Divilio LT, Patel B (2004) Combined anterior and posterior inguinal hernia repair: intermediate recurrence rates with three groups of surgeons. Hernia 8(3):203–207
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8(1):1–7
Rutkow IM (2003) The PerFix plug repair for groin hernias. Surg Clin North Am 83(5):1079–1098, vi
Robbins AW, Rutkow IM (1998) Mesh plug repair and groin hernia surgery. Surg Clin North Am 78(6):1007–1023, vi–vii
Amid PK, Shulman AG, Lichtenstein IL (1996) Open “tension-free” repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 162(6):447–453
Vironen J, Nieminen J, Eklund A, Paavolainen P (2006) Randomized clinical trial of Lichtenstein patch or Prolene Hernia System for inguinal hernia repair. Br J Surg 93(1):33–39
Nordin P, Zetterström H, Gunnarsson U, Nilsson E (2003) Local, regional, or general anaesthesia in groin hernia repair: multicentre randomised trial. Lancet 362(9387):853–858
Nordin P, Hernell H, Unosson M, Gunnarsson U, Nilsson E (2004) Type of anaesthesia and patient acceptance in groin hernia repair: a multicentre randomised trial. Hernia 8(3):220–225
Bay-Nielsen M, Perkins FM, Kehlet H; Danish Hernia Database (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233(1):1–7
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244(2):212–219
Bay-Nielsen M, Nilsson E, Nordin P, Kehlet H; Swedish Hernia Data Base the Danish Hernia Data Base (2004) Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 91(10):1372–1376
Acknowledgments
This study was partially sponsored by Bard Norden AB (Helsingborg, Sweden) and the Ethicon Division of Johnson & Johnson AB (Sollentuna, Sweden). Neither the principal investigator (JD) nor any other participants had any personal financial interests whatsoever in the outcome of the study. Preliminary results of the study have been presented at the Swedish Surgical Society Meetings in 2002, 2004 and 2007, and at the 26th and 29th International Congresses of the European Hernia Society Meetings in Prague, Czech Republic, 2004, and in Athens, Greece, 2007. The authors extend their gratitude to the excellent secretarial assistance of Helen Bredstenslien, Britt-Marie Ingmansson and Carina Bergendahl-Kristensson, all at the Frölunda Specialist Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dalenbäck, J., Andersson, C., Anesten, B. et al. Prolene Hernia System, Lichtenstein mesh and plug-and-patch for primary inguinal hernia repair: 3-year outcome of a prospective randomised controlled trial. Hernia 13, 121–129 (2009). https://doi.org/10.1007/s10029-008-0443-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0443-4