Abstract
Purpose
Surgical site infection (SSI) increases medical costs and prolongs hospitalization; however, there has been no multicenter study examining the socioeconomic effects of SSI after cardiovascular surgery in Japan.
Methods
A retrospective 1:1 matched, case-controlled study on hospital stay and health care expenditure after cardiovascular surgery was performed in four hospitals. Patients selected for the study had undergone coronary artery bypass grafting and/or valve surgery between April, 2006 and March, 2008. Data were obtained for 30 pairs of patients.
Results
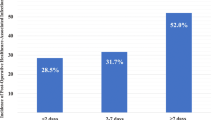
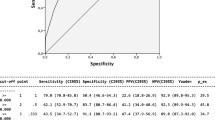
The mean postoperative stay for the SSI group was 49.1 days, being 3.7 times longer than that for the non-SSI group. The mean postoperative health care expenditure for the SSI group was ¥2,763,000 (US$27,630), being five times higher than that for the non-SSI group. Charges for drug infusion and hospitalization for inpatient care were significantly higher for the SSI group than for the non-SSI group. The increased health care expenditure was mainly attributed to the cost of antibiotics and antimicrobial agents.
Conclusion
SSI after cardiovascular surgery not only prolonged the length of hospital stay, but also increased medical expenditure. Thus, the prevention of SSI after cardiovascular surgery is of great socioeconomic importance.

Similar content being viewed by others
References
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–78.
Japan Nosocomial Infection Surveillance: http://www.nih-janis.jp/report/ssi.html.
Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e652–735.
Loop FD, Lytle BW, Cosgrove DM, Mahfood S, McHenry MC, Goormastic M, et al. J. Maxwell Chamberlain memorial paper. Sternal wound complications after isolated coronary artery bypass grafting: early and late mortality, morbidity, and cost of care. Ann Thorac Surg. 1990;49:179–86.
Milano CA, Kesler K, Archibald N, Sexton DJ, Jones RH. Mediastinitis after coronary artery bypass graft surgery. Risk factors and long-term survival. Circulation. 1995;92:2245–51.
Stahle E, Tammelin A, Bergstrom R, Hambreus A, Nyström SO, Hansson HE. Sternal wound complications—incidence, microbiology and risk factors. Eur J Cardiothorac Surg. 1997;11:1146–53.
Borger MA, Rao V, Weisel RD, Ivanov J, Cohen G, Scully HE, et al. Deep sternal wound infection: risk factors and outcomes. Ann Thorac Surg. 1998;65:1050–6.
Ridderstolpe L, Gill H, Granfeldt H, Ahlfeldt H, Rutberg H. Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardiothorac Surg. 2001;20:1168–75.
Abboud CS, Wey SB, Baltar VT. Risk factors for mediastinitis after cardiac surgery. Ann Thorac Surg. 2004;77:676–83.
Braxton JH, Marrin CA, McGrath PD, Morton JR, Norotsky M, Charlesworth DC, et al. 10-year follow-up of patients with and without mediastinitis. Semin Thorac Cardiovasc Surg. 2004;16:70–6.
Coskun D, Aytac J, Aydinli A, Bayer A. Mortality rate, length of stay and extra cost of sternal surgical site infections following coronary artery bypass grafting in a private medical centre in Turkey. J Hosp Infect. 2005;60:176–9.
Coello R, Charlett A, Wilson J, Ward V, Pearson A, Borriello P. Adverse impact of surgical site infections in English hospitals. J Hosp Infect. 2005;60:93–103.
Toumpoulis IK, Anagnostopoulos CE, Derose JJ Jr, Swistel DG. The impact of deep sternal wound infection on long-term survival after coronary artery bypass grafting. Chest. 2005;127:464–71.
Jenney AW, Harrington GA, Russo PL, Spelman DW. Cost of surgical site infections following coronary artery bypass surgery. ANZ J Surg. 2001;71:662–4.
Hollenbeak CS, Murphy DM, Koenig S, Woodward RS, Dunagan WC, Fraser VJ. The clinical and economic impact of deep chest surgical site infections following coronary artery bypass graft surgery. Chest. 2000;118:317–402.
Graf K, Ott E, Vonberg RP, Kuehn C, Haverich A, Chaberny IF. Economic aspects of deep sternal wound infections. Eur J Cardiothorac Surg. 2010;37:893–6.
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–97.
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725–30.
Upton A, Smith P, Roberts S. Excess cost associated with Staphylococcus aureus poststernotomy mediastinitis. N Z Med J. 2005;118:U1316.
Kusachi S, Kashimura N, Konishi T, Shimizu J, Kusunoki M, Oka M, et al. Length of stay and cost for surgical site infection after abdominal and cardiac surgery in Japanese hospitals: multi-center surveillance. Surg Infect (Larchmt). 2012;13:257–65.
Kashimura N, Kusachi S, Konishi T, Shimizu J, Kusunoki M, Oka M, et al. Impact of surgical site infection after colorectal surgery on hospital stay and medical expenditure in Japan. Surg Today. 2012;42:639–45.
State Medicaid Director Letter # 08-004 July 31, 2008. Centers for Medicare & State Operations.
Edwards FH, Engelman RM, Houck P, Shahian DM, Bridges CR. The Society of Thoracic Surgeons Practice Guideline Series: antibiotic prophylaxis in cardiac surgery. Part I: duration. Ann Thorac Surg. 2006;81:397–404.
Engelman R, Shahian D, Shemin R, Guy TS, Bratzler D, Edwards F, et al. The Society of Thoracic Surgeons Practice Guideline Series: antibiotic prophylaxis in cardiac surgery, Part II: antibiotic choice. Ann Thorac Surg. 2007;83:1569–76.
Imai-Kawata S, Fushimi K. Factors associated with adherence to prophylactic antibiotic therapy for elective general surgery in Japan. Int J Qual Health Care. 2011;23:167–72.
Gorwitz RJ, Kruszon-Moran D, McAllister SK, McQuillan G, McDougal LK, Fosheim GE, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001–2004. J Infect Dis. 2008;197:1226–34.
JANIS Annual Report 2012. http://www.nihjanis.jp/report/open_report/2011/3/1/ken_Open_Report_201100.pdf.
Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, et al. Survey of infections due to staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific Region for the SENTRY antimicrobial surveillance program, 1997–1999. Clin Infec Dis. 2001;32(Suppl. 2):S-114–32.
Kuwano H, Amano J, Yokomise H. Thoracic and cardiovascular surgery in Japan during 2010: annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2012;60:680–708.
Acknowledgments
We thank the researchers who provided the required information at the medical facilities that participated in this study, and the staff responsible for medical information and administration.
Conflict of interest
This study was carried out by the Clinical Trial Committee of the Japan Society for Surgical Infection supported by Johnson & Johnson KK. None of the authors has a conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kobayashi, J., Kusachi, S., Sawa, Y. et al. Socioeconomic effects of surgical site infection after cardiac surgery in Japan. Surg Today 45, 422–428 (2015). https://doi.org/10.1007/s00595-014-0969-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-0969-2