Abstract
Background
The Australian and New Zealand Audit of Surgical Mortality (ANZASM) National Report 2015 found that within the cohort of audited deaths, 85% were emergencies with acute life-threatening conditions, and by far, the most common procedures were laparotomy and colorectal procedures. Emergency laparotomy outcomes have shown improvement through audit and reporting in the UK. The purpose of this study was to determine the outcome of emergency laparotomy in the state of Victoria, Australia.
Method
The Dr Foster Quality Investigator (DFQI) database was interrogated for a set of Australian Classification of Health Intervention (ACHI) codes defined by the authors as representing an emergency laparotomy. The dataset included patients who underwent emergency laparotomy from July 2007 to July 2016 in all Victorian hospitals.
Results
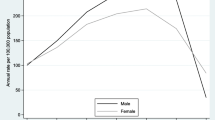
There were 23,115 emergency laparotomies conducted over 9 years in 66 hospitals. Inpatient mortality was 2036/23,115 (8.8%). Mortality in the adult population increased with age and reached 18.1% in those patients that were 80 years or older. 51.3% were females, and there was no significant difference in survival between genders. Patients with no recorded comorbidities had a mortality of 4.3%, whereas those with > 5 comorbidities had 19.3% mortality.
Conclusion
Administrative data accessed via a tool such as DFQI can provide useful population data to guide further evidence-based improvement strategies. The mortality for emergency laparotomy within Victorian hospitals is comparable, if not better than that seen in overseas studies. There is a need to continue routine audit of mortality rates and implement systems improvement where necessary.


Similar content being viewed by others
References
Al-Temimi MH, Griffee M, Enniss TM et al (2012) When is death inevitable after emergency laparotomy? Analysis of the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg 215:503–511
Saunders DI, Murray D, Pichel AC et al (2012) Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth 109:368–375
Azzam DG, Neo CA, Itotoh FE et al (2013) The Western Australian Audit of Surgical Mortality: outcomes from the first 10 years. Med J Aust 199:539–542
Beiles CB, Retegan C, Maddern GJ (2015) Victorian Audit of Surgical Mortality is associated with improved clinical outcomes. ANZ J Surg 85:803–807
Watters DA, Hollands MJ, Gruen RL et al (2015) Perioperative mortality rate (POMR): a global indicator of access to safe surgery and anaesthesia. World J Surg 39:856–864
Surgeons RACo (2016) Australian and New Zealand audit of surgical mortality national report 2015
Surgeons RACo (2016) Victorian audit of surgical mortality report 2015
Crebbin W, Beasley SW, Watters DA (2013) Clinical decision making: how surgeons do it. ANZ J Surg 83:422–428
Milnes S, Orford NR, Berkeley L et al (2015) A prospective observational study of prevalence and outcomes of patients with Gold Standard Framework criteria in a tertiary regional Australian Hospital. BMJ Support Palliat Care
Orford NR, Milnes SL, Lambert N et al (2016) Prevalence, goals of care and long-term outcomes of patients with life-limiting illness referred to a tertiary ICU. Crit Care Resusc 18:181–188
Tan BH, Mytton J, Al-Khyatt W et al (2016) A Comparison of mortality following emergency laparotomy between populations from New York State and England. Ann Surg
RCoA (2016) The second patient report of the national emergency laparotomy audit (NELA)
Collaborative G (2016) Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg 103:971–988
Patel AA, Singh K, Nunley RM et al (2016) administrative databases in orthopaedic research: pearls and pitfalls of big data. J Am Acad Orthop Surg 24:172–179
Statistics ABo Australian Demographic Statistics, cat. no. 3101.0 viewed 01 Mar 2017. http://www.abs.gov.au/AUSSTATS/abs@.nsf/allprimarymainfeatures/61D19DFBD033B48FCA257CA7000DCB16?opendocument
RCoA (2015) The first patient report of the national emergency laparotomy audit
Elixhauser A, Steiner C, Harris D et al (1998) Comorbidity measures for use with administrative data. MedCare 36:8–27
American College of Surgeons national surgical quality improvement program. http://site.acsnsqip.org/
The Doctor Foster Global Comparators Study. http://drfosterintelligence.co.uk/global-comparators/
The enhanced peri-operative care for high-risk patients (EPOCH) trial. http://www.epochtrial.org/epoch.php
Fletcher A, Worthington D (2009) What is a ‘generic’ hospital model?—a comparison of ‘generic’ and ‘specific’ hospital models of emergency patient flows. Health Care Manag Sci 12:374–391
Nagaraja V, Eslick GD, Cox MR (2014) The acute surgical unit model verses the traditional “on call” model: a systematic review and meta-analysis. World J Surg 38:1381–1387
Truskett P (2010) Acute surgery units: the future face of emergency surgery. ANZ J Surg 80:477–478
Raju RS, Guy GS, Majid AJ et al (2015) The Australian and New Zealand audit of surgical mortality-birth, deaths, and carriage. Ann Surg 261:304–308
Weiser TG, Haynes AB, Dziekan G et al (2010) Effect of a 19-item surgical safety checklist during urgent operations in a global patient population. Ann Surg 251:976–980
Peden CJ (2011) Emergency surgery in the elderly patient: a quality improvement approach. Anaesthesia 66:440–445
Wilson I, Paul Barrett M, Sinha A et al (2014) Predictors of in-hospital mortality amongst octogenarians undergoing emergency general surgery: a retrospective cohort study. Int J Surg 12:1157–1161
Stupart DA, Watters DA, Guest GD et al (2013) Dedicated emergency theatres improve service delivery and surgeons’ job satisfaction. ANZ J Surg 83:549–553
Author information
Authors and Affiliations
Corresponding author
Annex A: Australian classification of health interventions codes
Annex A: Australian classification of health interventions codes
These codes were including multiple editions (4th–7th) to cover the years included in the study.
Small bowel resection |
30375-09 Excision of Meckel’s diverticulum |
30405-02 Repair of incisional hernia with resection of strangulated intestine |
30405-05 Repair of other abdominal wall hernia with resection of strangulated intestine |
30565-00 Resection of small intestine with formation of stoma |
30566-00 Resection of small intestine with anastomosis |
Colonic resection with anastomosis |
30515-03 Ileocolic resection with anastomosis |
32003-00 Limited excision of large intestine with anastomosis |
32003-01 Right hemicolectomy with anastomosis |
32005-00 Subtotal colectomy with anastomosis |
32005-01 Extended right hemicolectomy with anastomosis |
32006-00 Left hemicolectomy with anastomosis |
32024-00 High anterior resection of rectum |
Division of adhesions |
30378-00 Division of abdominal adhesions |
Colonic resection with stoma |
30515-05 Ileocolic resection with formation of stoma |
32000-00 Limited excision of large intestine with formation of stoma |
32000-01 Right hemicolectomy with formation of stoma |
32004-00 Subtotal colectomy with formation of stoma |
32004-01 Extended right hemicolectomy with formation of stoma |
32006-01 Left hemicolectomy with formation of stoma |
32009-00 Total colectomy with ileostomy |
32030-00 Rectosigmoidectomy with formation of stoma |
Other laparotomy |
30375-01 Other enterostomy |
30375-04 Other colostomy |
30375-08 Reduction in intussusception of small intestine |
30375-11 Reduction in intussusception of large intestine |
30375-15 Gastrotomy with removal of foreign body |
30375-17 Reduction in volvulus of large intestine |
30375-18 Reduction in volvulus of small intestine |
30375-19 Other repair of small intestine |
30392-00 Debulking of intra-abdominal lesion |
30394-00 Drainage of intra-abdominal abscess, hematoma or cyst |
30402-00 Drainage of retroperitoneal abscess, hematoma or cyst |
30505-00 Control of bleeding peptic ulcer |
30509-00 Control of bleeding peptic ulcer by gastric resection |
30512-00 Gastric bypass |
30515-00 Gastro-enterostomy |
30515-01 Enterocolostomy |
30515-02 Enteroenterostomy |
30518-00 Partial distal gastrectomy with gastroduodenal anastomosis |
30518-01 Partial distal gastrectomy with gastrojejunal anastomosis |
30563-02 Repair of parastomal hernia |
30564-00 Strictureplasty of small intestine |
Exploratory laparotomy |
30373-00 Exploratory laparotomy Debridement and lavage of peritoneal cavity for gross intra peritoneal sepsis |
30396-00 Debridement and lavage of peritoneal cavity |
Perforated viscous |
30375-10 Suture of perforated ulcer |
30375-03 Enterotomy of small intestine |
30375-24 Suture of small intestine |
30375-25 Suture of laceration of large intestine |
Rights and permissions
About this article
Cite this article
Stevens, C.L., Brown, C. & Watters, D.A.K. Measuring Outcomes of Clinical Care: Victorian Emergency Laparotomy Audit Using Quality Investigator. World J Surg 42, 1981–1987 (2018). https://doi.org/10.1007/s00268-017-4418-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4418-4