Abstract
Purpose
To compare frequency and inter-reader agreement for LI-RADS v2014 major features at CT vs. MRI in pathology-proven cases of hepatocellular carcinoma.
Methods
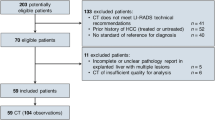
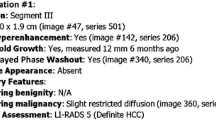
Pathology reports and imaging studies from patients having undergone liver transplant or hepatectomy for hepatocellular carcinoma were reviewed. Size, location, washout, and capsule appearance for each lesion were recorded by two radiologists. Cohen’s kappa and intraclass correlation coefficients (ICC) were calculated.
Results
One hundred and thirty-four patients with 184 tumors were reviewed. Seventy-seven percentage of lesions were imaged by CT and 23% by MRI. No lesions were evaluated with both modalities. Mean lesion diameter was 2.6 ± 1.3 cm (ICC = 0.92). Arterial phase hyperenhancement was seen in 86% of lesions (κ = 0.75). Washout was seen in 82% of studies (κ = 0.61). Arterial phase hyperenhancement and washout were seen equally at CT and MRI (p = 1.00 and 0.46, respectively). Capsule was infrequently observed (27%) but was seen more commonly at MRI (44%) than at CT (17%) with p = 0.002 and (κ = 0.56). Forty-seven percent of lesions with at least one prior study met LI-RADS criteria for threshold growth. The rates of LI-RADS categories 3, 4, and 5 were 9%, 37%, and 54%, respectively. More 1–2 cm LI-RADS 5 lesions were seen at MRI (43%) than at CT (8%), p = 0.01.
Conclusion
A combined LI-RADS 4/5 group was 91% sensitive for hepatocellular carcinoma. Arterial enhancement and washout were seen more frequently than capsule, the sole finding seen more frequently at MRI than at CT. Inter-reader reliability was substantial for arterial hyperenhancement and washout but moderate for capsule. Capsule remains an important finding in small arterially enhancing lesions (1–2 cm) which require a second major criterion to upgrade to a LI-RADS 5 lesion.




Similar content being viewed by others
References
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53(3):1020–1022. doi:10.1002/hep.24199
Wald C, Russo MW, Heimbach JK, et al. (2013) New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology 266(2):376–382. doi:10.1148/radiol.12121698
Practice guidelines for management of hepatocellular carcinoma (2009) 2009. Korean J Hepatol 15(3):391–423. doi:10.3350/kjhep.2009.15.3.391
European Association for the Study of the Liver (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56(4):908–943. doi:10.1016/j.jhep.2011.12.001
Omata M, Lesmana LA, Tateishi R, et al. (2010) Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatology international 4(2):439–474. doi:10.1007/s12072-010-9165-7
Kudo M, Izumi N, Kokudo N, et al. (2011) Management of hepatocellular carcinoma in Japan: Consensus-Based Clinical Practice Guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Digest Dis 29(3):339–364. doi:10.1159/000327577
Quality and safety resources: liver imaging–reporting and data system. Am Coll Radiol. http://www.acr.org/Quality-Safety/Resources/LIRADS. Accessed 16 Sep 2015
Freeman RB Jr, Wiesner RH, Harper A, et al. (2002) The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transplant 8(9):851–858. doi:10.1053/jlts.2002.35927
Freeman RB Jr, Gish RG, Harper A, et al. (2006) Model for end-stage liver disease (MELD) exception guidelines: results and recommendations from the MELD Exception Study Group and Conference (MESSAGE) for the approval of patients who need liver transplantation with diseases not considered by the standard MELD formula. Liver Transplant 12(12 Suppl 3):S128–S136. doi:10.1002/lt.20979
Sharma P, Balan V, Hernandez JL, et al. (2004) Liver transplantation for hepatocellular carcinoma: the MELD impact. Liver Transplant 10(1):36–41. doi:10.1002/lt.20012
Ioannou GN, Perkins JD, Carithers RL Jr (2008) Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology 134(5):1342–1351. doi:10.1053/j.gastro.2008.02.013
Burrel M, Llovet JM, Ayuso C, et al. (2003) MRI angiography is superior to helical CT for detection of HCC prior to liver transplantation: an explant correlation. Hepatology 38(4):1034–1042. doi:10.1053/jhep.2003.50409
Rode A, Bancel B, Douek P, et al. (2001) Small nodule detection in cirrhotic livers: evaluation with US, spiral CT, and MRI and correlation with pathologic examination of explanted liver. J Comput Assist Tomogr 25(3):327–336
Kim YK, Kim CS, Chung GH, et al. (2006) Comparison of gadobenate dimeglumine-enhanced dynamic MRI and 16-MDCT for the detection of hepatocellular carcinoma. AJR Am J Roentgenol 186(1):149–157. doi:10.2214/ajr.186.4_supplement.a149
Krinsky GA, Lee VS, Theise ND, et al. (2001) Hepatocellular carcinoma and dysplastic nodules in patients with cirrhosis: prospective diagnosis with MR imaging and explantation correlation. Radiology 219(2):445–454. doi:10.1148/radiology.219.2.r01ma40445
Sangiovanni A, Manini MA, Iavarone M, et al. (2010) The diagnostic and economic impact of contrast imaging techniques in the diagnosis of small hepatocellular carcinoma in cirrhosis. Gut 59(5):638–644. doi:10.1136/gut.2009.187286
Lim JH, Kim CK, Lee WJ, et al. (2000) Detection of hepatocellular carcinomas and dysplastic nodules in cirrhotic livers: accuracy of helical CT in transplant patients. AJR Am J Roentgenol 175(3):693–698. doi:10.2214/ajr.175.3.1750693
Fowler KJ, Karimova EJ, Arauz AR, et al. (2013) Validation of organ procurement and transplant network (OPTN)/united network for organ sharing (UNOS) criteria for imaging diagnosis of hepatocellular carcinoma. Transplantation 95(12):1506–1511. doi:10.1097/TP.0b013e31828eeab2
Petruzzi N, Mitchell D, Guglielmo F, et al. (2013) Hepatocellular carcinoma likelihood on MRI exams: evaluation of a standardized categorization system. Acad Radiol 20(6):694–698. doi:10.1016/j.acra.2013.01.016
Davenport MS, Khalatbari S, Liu PS, et al. (2014) Repeatability of diagnostic features and scoring systems for hepatocellular carcinoma by using MR imaging. Radiology 272(1):132–142. doi:10.1148/radiol.14131963
Furlan A, Marin D, Vanzulli A, et al. (2011) Hepatocellular carcinoma in cirrhotic patients at multidetector CT: hepatic venous phase versus delayed phase for the detection of tumour washout. Br J Radiol 84(1001):403–412. doi:10.1259/bjr/18329080
Cereser L, Furlan A, Bagatto D, et al. (2010) Comparison of portal venous and delayed phases of gadolinium-enhanced magnetic resonance imaging study of cirrhotic liver for the detection of contrast washout of hypervascular hepatocellular carcinoma. J Comput Assist Tomogr 34(5):706–711. doi:10.1097/RCT.0b013e3181e1a88e
Mazzaferro V, Regalia E, Doci R, et al. (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. New Engl J Med 334(11):693–699. doi:10.1056/nejm199603143341104
Yao FY, Ferrell L, Bass NM, et al. (2001) Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 33(6):1394–1403. doi:10.1053/jhep.2001.24563
Edge SBD, Compton CC, Fritz AG, Greene FL, Trotti A (2010) AJCC cancer staging handbook, 7th edn. Chicago: American Joint Committee on Cancer
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Study performed with approval from UCSF Committee on Human Research (IRB) approval.
Rights and permissions
About this article
Cite this article
Ehman, E.C., Behr, S.C., Umetsu, S.E. et al. Rate of observation and inter-observer agreement for LI-RADS major features at CT and MRI in 184 pathology proven hepatocellular carcinomas. Abdom Radiol 41, 963–969 (2016). https://doi.org/10.1007/s00261-015-0623-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0623-5