Abstract
Objective
To evaluate a simultaneous PET/MRI approach to imaging patients with neuroendocrine tumor using a combination of 68Ga-DOTA-TOC as a PET contrast agent and gadoxetate disodium as a hepatobiliary MRI contrast agent.
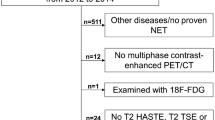
Materials and methods
Ten patients with neuroendocrine tumor with known or suspected hepatic disease were imaged using a 68Ga-DOTA-TOC PET/CT immediately followed by a 3.0T time-of-flight PET/MRI, using a combined whole body and liver specific imaging. The presence of lesions and DOTA-TOC avidity were assessed on CT, PET from PET/CT, diffusion weighted imaging, hepatobiliary phase imaging (HBP), and PET from PET/MRI. Maximum standardized uptake values (SUVmax) in hepatic lesions and nodal metastases were compared between PET/CT and PET/MRI, as were detection rates using each imaging approach.
Results
A total of 101 hepatic lesions were identified, 47 of which were DOTA-TOC avid and able to be individually measured on both PET/CT and PET/MRI. HBP imaging had a higher sensitivity for detection of hepatic lesions compared to CT or PET (99% vs. 46% and 64%, respectively; p values <0.001). There was a strong correlation between SUVmax of liver lesions obtained with PET/CT compared to PET/MR imaging (Pearson’s correlation = 0.91). For nodal disease, CT had a higher sensitivity compared to whole body MRI (p = 0.015), although PET acquired from PET/MRI detected slightly more lesions compared to PET from PET/CT.
Conclusions
A simultaneous PET/MRI using both 68Ga-DOTA-TOC and gadoxetate disodium was successful in whole body staging of patients with neuroendocrine tumor. HBP imaging had an increased detection rate for hepatic metastases.






Similar content being viewed by others

References
Yao JC, Hassan M, Phan A, et al. (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26(18):3063–3072
Wang SC, Fidelman N, Nakakura EK (2013) Management of well-differentiated gastrointestinal neuroendocrine tumors metastatic to the liver. Semin Oncol 40(1):69–74
Ruf J, Heuck F, Schiefer J, et al. (2010) Impact of Multiphase 68Ga-DOTATOC-PET/CT on therapy management in patients with neuroendocrine tumors. Neuroendocrinology. 91(1):101–109
Krenning EP, Kwekkeboom DJ, Bakker WH, et al. (1993) Somatostatin receptor scintigraphy with [111In-DTPA-D-Phe1]- and [123I-Tyr3]-octreotide: the Rotterdam experience with more than 1000 patients. Eur J Nucl Med 20(8):716–731
Yang J, Kan Y, Ge BH (2013) Diagnostic role of Gallium-68 DOTATOC and Gallium-68 DOTATATE PET in patients with neuroendocrine tumors: a meta-analysis. Acta Radiol 55(4):389–398
Buchmann I, Henze M, Engelbrecht S, et al. (2007) Comparison of 68Ga-DOTATOC PET and 111In-DTPAOC (Octreoscan) SPECT in patients with neuroendocrine tumours. Eur J Nucl Med Mol Imaging 34(10):1617–1626
Gabriel M, Decristoforo C, Kendler D, et al. (2007) 68Ga-DOTA-Tyr3-octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med 48(4):508–518
Dromain C, De Baere T, Lumbroso J, et al. (2005) Detection of liver metastases from endocrine tumors: a prospective comparison of somatostatin receptor scintigraphy, computed tomography, and magnetic resonance imaging. J Clin Oncol 23(1):70–78
Sankowski AJ, Ćwikla JB, Nowicki ML, et al. (2012) The clinical value of MRI using single-shot echoplanar DWI to identify liver involvement in patients with advanced gastroenteropancreatic-neuroendocrine tumors (GEP-NETs), compared to FSE T2 and FFE T1 weighted image after i.v. Gd-EOB-DTPA contrast enhancement. Med Sci Monit 18((5):MT33–MT40
Mayerhoefer ME, Ba-Ssalamah A, Weber M, et al. (2013) Gadoxetate-enhanced versus diffusion-weighted MRI for fused Ga-68-DOTANOC PET/MRI in patients with neuroendocrine tumours of the upper abdomen. Eur Radiol 23(7):1978–1985
Giesel FL, Kratochwil C, Mehndiratta A, et al. (2012) Comparison of neuroendocrine tumor detection and characterization using DOTATOC-PET in correlation with contrast enhanced CT and delayed contrast enhanced MRI. Eur J Radiol 81(10):2820–2825
Schreiter NF, Nogami M, Steffen I, et al. (2012) Evaluation of the potential of PET-MRI fusion for detection of liver metastases in patients with neuroendocrine tumours. Eur Radiol 22(2):458–467
Wollenweber SD, Ambwani S. Comparison of 4-class and continuous fat/water methods for whole-body, MR-based PET attenuation correction. IEEE Nuclear Science Symposiwn and Medical Imaging Conference Record. 2013 Jun 20:1–7
Wollenweber SD, Ambwani S. Evaluation of an atlas-based PET head attenuation correction using PET/CT & MR patient data. IEEE Nuclear Science Symposiwn and Medical Imaging Conference Record. 2012
Benndorf M, Schelhorn J, Dietzel M, Kaiser WA, Baltzer PAT (2012) Diffusion weighted imaging of liver lesions suspect for metastases: apparent diffusion coefficient (ADC) values and lesion contrast are independent from Gd-EOB-DTPA administration. Eur J Radiol 81(8):e849–e853
Bashir MR, Husarik DB, Ziemlewicz TJ, et al. (2012) Liver MRI in the hepatocyte phase with gadolinium-EOB-DTPA: does increasing the flip angle improve conspicuity and detection rate of hypointense lesions? J Magn Reson Imaging 35(3):611–616
Nagle SK, Busse RF, Brau AC, et al. (2012) High resolution navigated three-dimensional T1-weighted hepatobiliary MRI using gadoxetic acid optimized for 1.5 Tesla. J Magn Reson Imaging 36(4):890–899
Beiderwellen KJ, Poeppel TD, Hartung-Knemeyer V, et al. (2013) Simultaneous 68Ga-DOTATOC PET/MRI in patients with gastroenteropancreatic neuroendocrine tumors: initial results. Invest Radiol 48(5):273–279
Chandarana H, Heacock L, Rakheja R, et al. (2013) Pulmonary nodules in patients with primary malignancy: comparison of hybrid PET/MR and PET/CT imaging. Radiology 268(3):874–881
Acknowledgements
Grant support from Wylie J. Dodds Research Award, Society of Abdominal Radiology, GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hope, T.A., Pampaloni, M.H., Nakakura, E. et al. Simultaneous 68Ga-DOTA-TOC PET/MRI with gadoxetate disodium in patients with neuroendocrine tumor. Abdom Imaging 40, 1432–1440 (2015). https://doi.org/10.1007/s00261-015-0409-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0409-9