Abstract
Purpose
The aim of the study was to determine the accuracy, reproducibility, and improvement in the clinical workflow of a semiautomatic computed tomography (CT) virtual surgical planning program in estimating graft volume using actual graft weight as a standard of reference in living liver donors.
Materials and methods
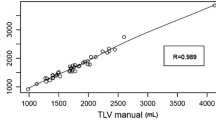
This retrospective study was approved by our Institutional Review Board and the requirement for informed consent was waived. A total of 105 liver donor candidates who underwent preoperative liver CT were reviewed. Volumes of the whole liver (V T), four hepatic segments, and predicted volumes of the hepatic graft (V pred) were obtained using a semiautomatic analysis program by radiologists and a conventional manual volumetry program by surgeons. Intraobserver and interobserver agreements of V T and V pred were assessed using intraclass correlation coefficients (ICCs). V pred was also compared to the actual graft weight (W act) and analysis times were recorded. In addition, potential vascular complications were assessed using the surgical planning function of the software.
Results
The mean processing time of hepatic volumetry, segmentation, and surgical planning using software was significantly shorter than that using manual volumetry (175.9 ± 46.6 vs. 916.6 ± 52.8 s, P < 0.001). V T and V pred obtained using the semiautomatic analysis program showed significant intra and interobserver agreements (ICC = 0.98–0.99), and V pred showed strong correlation with W act (r = 0.83–0.86, P < 0.0001). Furthermore, image review using the liver analysis program detected 80% (4/5) vascular complications.
Conclusion
Liver volumetry and estimation of graft volume using liver analysis software provided good accuracy and excellent reproducibility in a short time than manual volumetry method and was useful for identifying vascular complications.




Similar content being viewed by others
References
Adam R, McMaster P, O’Grady JG, et al. (2003) Evolution of liver transplantation in Europe: report of the European Liver Transplant Registry. Liver Transpl 9:1231–1243
Mazzaferro V, Regalia E, Doci R, et al. (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334:693–700
Trotter JF, Wachs M, Everson GT, Kam I (2002) Adult-to-adult transplantation of the right hepatic lobe from a living donor. N Engl J Med 346:1074–1082
Kiuchi T, Kasahara M, Uryuhara K, et al. (1999) Impact of graft size mismatching on graft prognosis in liver transplantation from living donors1, 2. Transplantation 67:321–327
Brown RS Jr, Russo MW, Lai M, et al. (2003) A survey of liver transplantation from living adult donors in the United States. N Engl J Med 348:818–825
Akabayashi A, Slingsby BT, Fujita M (2004) The first donor death after living-related liver transplantation in Japan. Transplantation 77:634
Morgan GR, Diflo T, John D, Teperman L (2001) Selection and imaging of the living liver donor. Curr Opin Organ Transplant 6:350–354
Asakuma M, Fujimoto Y, Bourquain H, et al. (2007) Graft selection algorithm based on congestion volume for adult living donor liver transplantation. Am J Transplant 7:1788–1796
Lee S, Park K, Hwang S, et al. (2001) Congestion of right liver graft in living donor liver transplantation. Transplantation 71:812–814
Dello SA, van Dam RM, Slangen JJ, et al. (2007) Liver volumetry plug and play: do it yourself with ImageJ. World J Surg 31:2215–2221
van der Vorst JR, van Dam RM, van Stiphout RS, et al. (2010) Virtual liver resection and volumetric analysis of the future liver remnant using open source image processing software. World J Surg 34:2426–2433
Kamel IR, Kruskal JB, Warmbrand G, et al. (2001) Accuracy of volumetric measurements after virtual right hepatectomy in potential donors undergoing living adult liver transplantation. Am J Roentgenol 176:483–487
Hermoye L, Laamari-Azjal I, Cao Z, et al. (2005) Liver segmentation in living liver transplant donors: comparison of semiautomatic and manual methods 1. Radiology 234:171–178
Bourquain H, Schenk A, Link F, et al. (2002) HepaVision2—a software assistant for preoperative planning in living-related liver transplantation and oncologic liver surgery. In: Lemke HU, Vannier MW, Imamura K (eds) CARS 2002 Computer Assisted Radiology and Surgery. Amsterdam: Springer, pp 341–346
Couinaud C (1957) Le foie: études anatomiques et chirurgicales. Paris: Masson
Zahel T, Wildgruber M, Ardon R, et al. (2013) Rapid assessment of liver volumetry by a novel automated segmentation algorithm. J Comput Assist Tomogr 37:577–582
Hiroshige S, Shimada M, Harada N, et al. (2003) Accurate preoperative estimation of liver-graft volumetry using three-dimensional computed tomography. Transplantation 75:1561–1564
Terzopoulos D, Waters K (1990) Physically-based facial modelling, analysis, and animation. J Vis Comput Anim 1:73–80
McInerney T, Terzopoulos D (1996) Deformable models in medical image analysis: a survey. Med Image Anal 1:91–108
Costa MJ, Delingette H, Novellas S, Ayache N (2007) Automatic segmentation of bladder and prostate using coupled 3D deformable models. In: Medical Image Computing and Computer-Assisted Intervention—MICCAI 2007. Springer, Berlin, pp 252–260
Olabarriaga SD, Rouet J-M, Fradkin M, Breeuwer M, Niessen WJ (2005) Segmentation of thrombus in abdominal aortic aneurysms from CTA with nonparametric statistical grey level appearance modeling. IEEE Trans Med Imaging 24:477–485
Lesage D, Angelini ED, Bloch I, Funka-Lea G (2009) A review of 3D vessel lumen segmentation techniques: Models, features and extraction schemes. Med Image Anal 13:819–845
Suh KS, Kim SH, Kim SB, Lee HJ, Lee KU (2002) Safety of right lobectomy in living donor liver transplantation. Liver Transpl 8:910–915
Yonemura Y, Taketomi A, Soejima Y, et al. (2005) Validity of preoperative volumetric analysis of congestion volume in living donor liver transplantation using three-dimensional computed tomography. Liver Transpl 11:1556–1562
Zou KH, Tuncali K, Silverman SG (2003) Correlation and simple linear regression 1. Radiology 227:617–628
Nakayama Y, Li Q, Katsuragawa S, et al. (2006) Automated hepatic volumetry for living related liver transplantation at multisection ct1. Radiology 240:743–748
Lemke A-J, Brinkmann MJ, Schott T, et al. (2006) Living donor right liver lobes: preoperative CT volumetric measurement for calculation of intraoperative weight and volume 1. Radiology 240:736–742
Karlo C, Reiner C, Stolzmann P, et al. (2010) CT-and MRI-based volumetry of resected liver specimen: comparison to intraoperative volume and weight measurements and calculation of conversion factors. Eur J Radiol 75:e107–e111
Van Thiel D, Hagler N, Schade R, et al. (1985) In vivo hepatic volume determination using sonography and computed tomography. Validation and a comparison of the two techniques. Gastroenterology 88:1812–1817
Bassignani MJ, Fulcher AS, Szucs RA, et al. (2001) Use of imaging for living donor liver transplantation 1. Radiographics 21:39–52
Lee MW, Lee JM, Lee JY, et al. (2006) Preoperative evaluation of the hepatic vascular anatomy in living liver donors: comparison of CT angiography and MR angiography. J Magn Reson Imaging 24:1081–1087
Radtke A, Sotiropoulos GC, Molmenti EP, et al. (2010) Computer-assisted surgery planning for complex liver resections: when is it helpful? A single-center experience over an 8-year period. Ann Surg 252:876–883
Kumamoto K, Mizuno S, Kuriyama N et al (2012) Postoperative liver dysfunction in living donors after left-sided graft hepatectomy: portal venous occlusion of the medial segment after lateral segmentectomy and hepatic venous congestion after left lobe hepatectomy. In: Transplantation proceedings. Elsevier, pp 332–337
Yamanaka J, Saito S, Fujimoto J (2007) Impact of preoperative planning using virtual segmental volumetry on liver resection for hepatocellular carcinoma. World J Surg 31:1249–1255
Lang H, Radtke A, Hindennach M, et al. (2005) Impact of virtual tumor resection and computer-assisted risk analysis on operation planning and intraoperative strategy in major hepatic resection. Arch Surg 140:629–638
Fasel JH (2008) Portal venous territories within the human liver: an anatomical reappraisal. Anat Rec 291:636–642
Takamoto T, Hashimoto T, Ogata S, et al. (2013) Planning of anatomical liver segmentectomy and subsegmentectomy with 3-dimensional simulation software. Am J Surg 206:530–538
Acknowledgment
We thank Chris Woo, B.A. (USA) for his editorial assistant, and Youngmi Chun, B.A. (Philips, Korea) for her technical support.
Conflict of interest
J.H.Y. No relevant conflicts of interest to disclose. J.M.L. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: Grants from Bayer Healthcare, Guerbet, and GE Healthcare. J.H.J. No relevant conflicts of interest to disclose. K.S.S. No relevant conflicts of interest to disclose. K.W.L. No relevant conflicts of interest to disclose. N.J.Y. No relevant conflicts of interest to disclose. P.C. Employee of Philips Healthcare. J.K.H. No relevant conflicts of interest to disclose. B.I.C. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: consultant of Samsung electronics (past).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yoon, J.H., Lee, J.M., Jun, J.H. et al. Feasibility of three-dimensional virtual surgical planning in living liver donors. Abdom Imaging 40, 510–520 (2015). https://doi.org/10.1007/s00261-014-0231-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0231-9