Abstract
Aims/hypothesis
We aimed to evaluate the link between severe hypoglycaemia and domain-specific cognitive decline, smaller brain volumes and dementia in adults with type 2 diabetes, which so far has been relatively poorly characterised.
Methods
We included participants with diagnosed diabetes from the community-based Atherosclerosis Risk in Communities (ARIC) study. At the participants’ fifth study visit (2011–2013), we examined the cross-sectional associations of severe hypoglycaemia with cognitive status, brain volumes and prior 15 year cognitive decline. We also conducted a prospective survival analysis of incident dementia from baseline, visit 4 (1996–1998), to 31 December 2013. Severe hypoglycaemia was identified, using ICD-9 codes, from hospitalisations, emergency department visits and ambulance records. Prior cognitive decline was defined as change in neuropsychological test scores from visit 4 (1996–1998) to visit 5 (2011–2013). At visit 5, a subset of participants underwent brain MRIs. Analyses were adjusted for demographics, APOE genotype, use of diabetes medication, duration of diabetes and glycaemic control.
Results
Among 2001 participants with diabetes at visit 5 (mean age 76 years), a history of severe hypoglycaemia (3.1% of participants) was associated with dementia (vs normal cognitive status): OR 2.34 (95% CI 1.04, 5.27). In the subset of participants who had undergone brain MRI (n = 580), hypoglycaemia was associated with smaller total brain volume (−0.308 SD, 95% CI −0.612, −0.004). Hypoglycaemia was nominally associated with a 15 year cognitive change (−0.14 SD, 95% CI −0.34, 0.06). In prospective analysis (n = 1263), hypoglycaemia was strongly associated with incident dementia (HR 2.54, 95% CI 1.78, 3.63).
Conclusions/interpretation
Our results demonstrate a strong link between severe hypoglycaemia and poor cognitive outcomes, suggesting a need for discussion of appropriate diabetes treatments for high-risk older adults.
Similar content being viewed by others

Introduction
The link between hypoglycaemia and cognitive function is complex but of great importance for the treatment of diabetes in both young and old adults [1, 2]. The short-term cognitive effects of hypoglycaemia are clear: even brief or mild hypoglycaemia causes symptoms of confusion and cognitive difficulties [3]. Although cognition appears to improve within an hour of restoration of normal blood glucose levels [3], there is concern about lasting brain damage, given case reports of brain abnormalities seen on diffusion-weighted imaging during hypoglycaemic coma [4, 5]. It is, however, unknown whether less severe and recurrent episodes of hypoglycaemia can produce permanent brain damage.
Some epidemiological studies have linked severe hypoglycaemia, defined as hypoglycaemia requiring assistance, with incident dementia, suggesting that hypoglycaemia may have long-term consequences for the brain [6,7,8]. Other longitudinal studies have, however, not demonstrated a consistent association between severe hypoglycaemia and subsequent cognitive decline, as measured by neurocognitive testing [9,10,11]. This raises questions about the mechanisms connecting hypoglycaemia to dementia, as a diagnosis of dementia is defined by loss of cognitive abilities resulting in impaired functioning in regular activities of daily life [12]. Additionally, there may be a bi-directional association between severe hypoglycaemia and cognitive function [7, 9, 13,14,15,16]: several studies have shown that poor cognitive function and cognitive decline are associated with incident hypoglycaemia, probably mediated in part by an impairment of diabetes self-management [14,15,16]. Indeed, individuals with dementia have a high risk of hypoglycaemia [7, 9, 13, 17]. This raises the possibility that cognitive decline before, or concurrent with, an episode of hypoglycaemia could in part explain the observed association between hypoglycaemia and subsequent dementia.
The overarching objective of our study was to evaluate comprehensively the association of severe hypoglycaemia with cognitive measures in a community-based population of adults with type 2 diabetes. By examining both dementia and cognitive decline in the same study population, we hoped to clarify the complex interplay between hypoglycaemia, cognitive decline and dementia. By examining domain-specific cognitive decline, we hoped to determine whether deficits associated with hypoglycaemia had a different signature from those associated with hyperglycaemia, which typically most strongly affect the executive function domain [18].
Our specific aims were: (1) to describe the prevalence of cognitive impairment and dementia in old age among those with and without a history of severe hypoglycaemia (‘cross-sectional cognitive status’ analysis); (2) to compare total and regional brain volumes measured by MRI among those with and without a history of severe hypoglycaemia (‘cross-sectional brain MRI subset’); (3) to determine whether a history of severe hypoglycaemia was associated with greater domain-specific cognitive decline (‘prior cognitive decline’ analysis); and (4) to determine the magnitude of the association of severe hypoglycaemia with incident dementia in a prospective survival analysis (‘prospective incident dementia’ analysis).
Methods
Study population
The Atherosclerosis Risk in Communities (ARIC) study enrolled 15,792 participants in 1987–1989 from four US communities: Jackson, MI; Forsyth County, NC; Washington County, MD; and selected suburbs of Minneapolis, MN [19]. Since baseline, participants have attended up to six study visits. The present study included only those participants with diagnosed diabetes by self-report of diagnosis or diabetes medication use. We identified individuals with possible type 1 diabetes as those who reported only insulin use (with no oral medication) at all study visits. Up to 34 individuals in each analysis had possible type 1 diabetes; as exclusion of these participants did not change the results, we retained them in our final analysis.
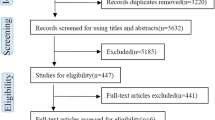
For the ‘cross-sectional cognitive status’, ‘cross-sectional brain MRI subset’ and ‘prior cognitive decline’ analyses, participants were selected from visit 5 (2011–2013) to provide final analytical samples of 2001, 580 and 1755 individuals, respectively. The ‘prospective incident dementia’ analysis included 1263 participants; the baseline was visit 4 (1996–1998), with follow-up to the end of 2013 (see electronic supplementary material [ESM] Fig. 1).
All ARIC participants gave their informed written consent, and institutional review board approval was obtained at all study sites.
Severe hypoglycaemia
Severe hypoglycaemic episodes were identified from hospitalisations, emergency department visits and ambulance calls by a widely used algorithm that employs primary position ICD-9 codes (www.icd9data.com/2007/Volume1) [20]. Hospitalisation records were available from two sources: (1) active surveillance, which captures all hospitalisations from local hospitals and also includes hospital records for ARIC participants who report hospitalisations outside the local catchment area, which has been available since visit 1 (1987–1989) [19]; and (2) linkage to Medicare claims for hospitalisations among participants enrolled in Medicare, which has been available since 1991. Emergency department visits and ambulance calls were identified from outpatient claims for those enrolled in Medicare fee-for-service Part B (88% of participants). Severe hypoglycaemic events were ascertained up to 31 December 2013.
Cognitive status: mild cognitive impairment and dementia
Assessment of cognitive status (normal, mild cognitive impairment or dementia) was based on available cognitive test scores from visits 2 (1990–1992), 4 (1996–1998) and 5 (2011–2013), the Clinical Dementia Rating (CDR), based on interviews with participants and informants, the Modified Telephone Interview for Cognitive Status (TICS), hospitalisation records and death certificates [21]. Diagnoses were standardised using an algorithm, with review by a panel of experts, who overrode the algorithm if indicated by their clinical judgement. For the analysis of incident dementia, a date of dementia diagnosis was assigned as the date of hospitalisation with a dementia ICD-9 code or, if no hospitalisation with dementia occurred, the first date of detection via the TICS or CDR, or visit 5 [22]. Follow-up ascertainment of dementia was complete up to 31 December, 2013.
Brain volumes
Brain volumes were measured by MRI (3 Tesla; Siemens, various models) in a substudy at visit 5 of 1978 participants. Detailed selection criteria are described elsewhere [23]. In brief, participants who had undergone previous brain MRIs in 2004–2006 or showed cognitive impairment at visit 5 were invited to participate in the substudy, as was a 10% random sample of cognitively normal participants [23]. Weights were created by the ARIC Coordinating Center to make the sample generalisable to visit 5 attendees [24]. We examined the total brain volume and the volumes of the frontal, temporal, occipital and parietal lobes, hippocampus, deep grey matter and Alzheimer’s disease signature region (defined as the total volume of the hippocampus, precuneus, cuneus and parahippocampal, entorhinal and inferior parietal lobules).
Latent factor z scores for cognitive domains
To examine cognitive decline, we calculated changes in neuropsychological test scores from visit 4 (1996–1998) to visit 5 (2011–2013). All participants who attended these two visits were administered the digit symbol substitution test, the word fluency test and the delayed word recall test. Seven additional tests were conducted at visit 5. To compare cognitive function across study visits while using all the cognitive tests administered at visit 5, Gross et al derived factor scores using confirmatory factor analysis for each cognitive domain [25]. At visit 5, the executive function domain factor score was based on the digit symbol substitution test, digit span backwards test and trail-making parts A and B. The language domain was based on the phonemic fluency test, the Boston naming test and the animal naming test. The memory domain included the delayed word recall test, incidental learning from the digit symbol substitution test, and the logical memory test parts 1 and 2. Factor scores were standardised to mean of 0 and SD of 1.
Statistical analysis
For the cross-sectional cognitive status analysis, we calculated the age-adjusted prevalence of normal cognitive function, mild cognitive impairment and dementia at visit 5 in participants with and without a history of severe hypoglycaemia (ESM Fig. 2). We also used multinomial logistic regression to compare the odds of having mild cognitive impairment or dementia by history of severe hypoglycaemia.
In the cross-sectional brain MRI subset analysis, we used linear regression to examine the association of a history of severe hypoglycaemia with current brain volume. All analyses were adjusted for total intracranial volume and an interaction term between sex and total intracranial volume. The MRI results were weighted to the original sample of attendees at visit 5 using the probability of selection for inclusion in the brain MRI substudy [23, 24].
For the analysis of prior cognitive decline, we evaluated the association of any severe hypoglycaemia between visit 4 (1996–1998) and visit 5 (2011–2013) with cognitive change over the same 15 year time period. We conducted linear regression, using the difference between factor scores at visits 5 and 4 as the outcome, for global cognitive function and each cognitive domain (executive function, language and memory).
To provide context for the results, we compared the magnitude of the association for hypoglycaemia with that for age from the same model. For example, if our model found that hypoglycaemia was associated with a 0.20 SD decline, and age was associated with a 0.05 SD decline (per year), hypoglycaemia would be analogous to a 4 year difference in age, for example the average difference in cognitive performance of a 76-year-old compared with an 80-year-old individual [18].
For the prospective incident dementia analysis, we used a Cox regression model for the outcome of incident dementia, with severe hypoglycaemia as a time-varying exposure, conceptualised as either ‘no history of severe hypoglycaemia’ or ‘history of severe hypoglycaemia’. At baseline (visit 4), we classified all individuals as ‘no history of severe hypoglycaemia’ unless a history of severe hypoglycaemia was present (n = 16). Throughout follow-up, when a participant experienced an episode of severe hypoglycaemia, all their person-time after that event was classified as exposed (‘history of severe hypoglycaemia’). Participants stopped contributing time to the analysis when they developed dementia or died, or on 31 December 2013, whichever occurred first. The assumption of proportional hazards was verified by inspection of loge negative loge survival curves. Because HbA1c was not measured at visit 4, the baseline for this analysis, we adjusted for fructosamine as a measure of glycaemic control. The results were similar using HbA1c concentrations from a visit 6 years previously.
We ran a series of three models for each cognitive outcome. Model 1 was adjusted for demographics only: age, sex and race-centre (two groups of black individuals, from Jackson and Forsyth, and three groups of white participants, from Forsyth, Minneapolis suburbs and Washington County). Model 2 was adjusted for all variables in model 1 plus APOE ε4 alleles (0 or ≥1 alleles) and education level (less than high school, high school graduate or some college education). Model 3 was adjusted for all variables in model 2 plus HbA1c concentration, duration of diabetes and use of diabetes medication (none, any insulin use, sulfonylureas without insulin or only non-sulfonylurea oral medications). Due to small sample size in the cross-sectional brain MRI subset, we used the same series of models described above, but used race rather than race-centre, and insulin use (yes/no) instead of the four medication categories. In the prospective incident dementia analysis, we also included model 4, which was additionally adjusted for systolic blood pressure, use of antihypertensive medication, albuminuria and low eGFR (<60 ml min−1 1.73 m−2), as these factors are associated with incident dementia and may also be associated with hypoglycaemia [16, 22, 26, 27].
All analyses were conducted using Stata/SE version 13.1 (StataCorp, College Station, TX, USA).
Results
Cross-sectional cognitive status
Of the 2001 participants with diagnosed diabetes, 3.1% (n = 63) had a history of severe hypoglycaemia by visit 5. Individuals with a history of severe hypoglycaemia had a substantially longer duration of diabetes and were more likely to use insulin. Additionally, they were, on average, older and more likely to be black, to have had less education and to have a greater number of APOE ε4 alleles (Table 1). The median time between hypoglycaemia and visit 5 was 5.6 years (25th and 75th percentiles, 2.3 and 8.1 years).
Age-adjusted cognitive status was strongly associated with a history of severe hypoglycaemia (Fig. 1). After multivariable adjustment, participants with a history of severe hypoglycaemia were significantly more likely to have dementia than normal cognitive function (OR 2.34, 95% CI 1.04, 5.27, model 3). Comparing mild cognitive impairment with normal cognitive function, the association with history of severe hypoglycaemia was evident but not statistically significant after adjustment (OR 1.50, 95% CI 0.82, 2.75, model 3).
Age-adjusted prevalence and 95% CI for mild cognitive impairment or dementia, with ORs, compared with normal cognitive status, by history of severe hypoglycaemia at visit 5 in the cross-sectional cognitive status analysis (n = 2001); 63 participants had a history of hypoglycaemia. White bars, no hypoglycaemia; grey bars, history of severe hypoglycaemia. Hypoglycaemia OR for cognitive impairment vs normal cognitive status: 1.50 (95% CI 0.82, 2.75). Hypoglycaemia OR for dementia vs normal cognitive status: 2.34 (95% CI 1.04, 5.27). ORs were adjusted for age, sex, race-centre, education, any APOE ε4 alleles, diabetes duration, diabetes medication and HbA1c concentration (model 3). Prevalence of normal cognitive status was 70% in those without hypoglycaemia, and 53% in those with hypoglycaemia
As a sensitivity analysis, we examined the prevalence of dementia among participants who did not attend visit 5. As expected, the prevalence of dementia was higher among those who did not attend visit 5 compared with those who did (14.5% vs 5.1%, respectively, in individuals without hypoglycaemia). The hypoglycaemia OR for dementia was slightly lower in those who did not attend visit 5 (OR 1.82, 95% CI 1.15, 2.87) compared with those who did attend it (OR 2.36, 95% CI 1.26, 4.44), adjusting for age, sex and race-centre.
Cross-sectional brain MRI substudy
In the brain MRI substudy (n = 580), 2.1% of participants (n = 12) had a history of severe hypoglycaemia. The time between hypoglycaemia and brain MRI was a median of 5.7 years (range 1.0–12.0 years). After adjustment, severe hypoglycaemia was associated with smaller total brain volume (−0.308 SD, 95% CI −0.612, −0.004, model 3; Table 2), equivalent to 31 cm3 (ESM Table 1) or analogous to a difference in age of 6.8 years (Table 2). A history of severe hypoglycaemia was also associated with a smaller frontal lobe volume (−0.385 SD, 95% CI −0.766, −0.004, model 3). Associations for other brain regions were weaker or absent.
Prior cognitive decline
Among the 1755 participants in the analysis of prior cognitive decline, 2.8% (n = 50) had a history of severe hypoglycaemia. Individuals with severe hypoglycaemia had greater prior cognitive decline (global factor score) than those without severe hypoglycaemia in the minimally adjusted model (−0.20 SD, 95% CI −0.39, −0.01, model 1; Table 3). After further adjustment, severe hypoglycaemia was no longer significantly associated with cognitive decline (−0.14 SD, 95% CI −0.34, 0.06, model 3), but the point estimate remained sizeable and was analogous to the difference in cognitive performance of two individuals differing in age by 4.6 years. Similarly, hypoglycaemia was not statistically significantly associated with domain-specific cognitive decline, but adjusted point estimates were large.
In sensitivity analyses, we additionally adjusted for the Center for Epidemiologic Studies Depression scale, albuminuria, hypertension and percentage weight change from visit 4 to visit 5. Although many of these variables were strongly associated with cognitive decline, they did not notably attenuate the association between hypoglycaemia and cognitive decline, probably because they were acting independently, rather than via hypoglycaemia, on cognitive decline. In a separate sensitivity analysis, we modelled the change in z scores of the three neuropsychological tests measured at both visits (delayed word recall, word fluency and digit symbol substitution), the results being similar (ESM Table 2).
Prospective incident dementia
Of 1263 participants with diabetes at visit 4 (1996–1998; mean age 64 years), 15.5% (n = 196) experienced an episode of severe hypoglycaemia until the end of 2013. Median follow-up time was 13.9 years. Individuals who experienced severe hypoglycaemia were more likely to be older and black, and to have lower cognitive scores, at visit 4 (ESM Table 3).
The incidence of dementia following an episode of severe hypoglycaemia was approximately five times greater than the incidence in the absence of severe hypoglycaemia (with severe hypoglycaemia, 51.3 per 1000 person-years, 95% CI 38.7, 68.1; without severe hypoglycaemia, 9.7 per 1000 person-years, 95% CI 8.2, 11.4; Table 4). After adjustment, severe hypoglycaemia was associated with a two and a half times greater risk of dementia, which was only minimally attenuated by adjustment (model 3, HR 2.54, 95% CI 1.78, 3.63; Table 4). Among the 48 participants with hypoglycaemia and subsequent dementia, the median time between these events was 3.5 years (25th and 75th percentiles 1.2 and 7.2 years).
When stratifying by baseline (visit 4) cognitive function, we found a statistically significant effect modification (p for interaction = 0.004). In the lower two tertiles of cognitive function, hypoglycaemia was not associated with incident dementia, whereas in the highest tertile of cognitive function, hypoglycaemia was associated with an almost five times higher risk of dementia (model 4; lowest tertile, HR 1.45, 95% CI 0.88, 2.41; highest tertile, HR 4.97; 95% CI 2.08, 11.89; ESM Table 4).
Discussion
Our study documents the substantial cognitive deficits that accompany severe hypoglycaemia among older adults with diabetes. Among participants with a history of severe hypoglycaemia in this community-based study of older adults (mean age 76 years), approximately half had either mild cognitive impairment or dementia. The adjusted prevalence of dementia was approximately two times higher in individuals with vs without a history of severe hypoglycaemia. With respect to total brain volume, the deficits associated with hypoglycaemia were analogous to an age difference of 7 years. Because of the nature of our study design, we cannot determine whether these deficits occurred before or after a hypoglycaemic event, but it is clear that individuals with a history of hypoglycaemia have a high burden of cognitive dysfunction.
To our knowledge, this is the first community-based cohort study to find smaller brain volumes in individuals with a history of severe hypoglycaemia. Although there have been case reports documenting imaging abnormalities during hypoglycaemic comas [4, 5], there has been only one other epidemiological inquiry using brain MRIs in type 2 diabetes [28]. The Action to Control Cardiovascular Disease Memory in Diabetes MRI substudy measured brain volumes at baseline and 40 months. The investigators found that individuals with severe hypoglycaemia had significantly less brain atrophy over 40 months than those without severe hypoglycaemia [28]. Additionally, there was no difference in change in the volume of abnormal white matter. Although the authors concluded that the brain was resilient to hypoglycaemia insults when hypoglycaemia did not lead to a coma [28], it is worth noting that the average age was 10 years younger than in our study and that a 40 month follow-up period may be insufficiently short.
Our region-specific brain volume results did not, however, correspond to our expectations. We found no difference in hippocampal volume in terms of history of severe hypoglycaemia, although previous studies have shown that neurones in the hippocampus are particularly vulnerable to hypoglycaemia [29]. Similarly, we detected a difference in the volume of the prefrontal region, which undergoes hyperperfusion during hypoglycaemia to prevent damage [3]. It is therefore unclear whether the observed differences in brain volume are due to severe hypoglycaemia, or whether the brain atrophy pre-dated the hypoglycaemic episode. The difference in total brain volume was large (0.308 SD); a previous ARIC study of the same brain MRI subset found a 0.20 SD difference in total brain volume between people with diabetes who had HbA1c ≥53mmol/mol (7%) compared with those with normoglycaemia (HbA1c <39 mmol/mol [5.7%]) [30].
We found a strong prospective association between severe hypoglycaemia and incident dementia, with a larger HR than seen in previous studies [6,7,8]. We also found a significant interaction in terms of baseline cognitive function, in that hypoglycaemia was associated with incident dementia among participants with high, but not low, cognitive function at baseline. Other studies have either excluded participants with low baseline cognitive function [7] or have not applied neurocognitive testing at baseline [6, 8]. It is possible that, as hypoglycaemia is more frequent among individuals with low cognitive function [14,15,16], individuals with high baseline cognitive function only have severe hypoglycaemia after substantial cognitive decline, nearing dementia. Alternatively, individuals with low baseline cognitive function may have a higher mortality rate, precluding them from developing dementia. Further studies are needed to investigate this finding.
Similar to other studies [9,10,11], we found that severe hypoglycaemia was not robustly associated with cognitive decline, although, like other studies, our study may have been underpowered. A study of older Australian adults found no association between prior hypoglycaemia and subsequent 18 month cognitive decline, but only 14 people had prior hypoglycaemia [9]. A Scottish study in which 77 of 816 participants reported previous hypoglycaemia found a significantly greater 4 year decline on one out of seven neurocognitive tests [10]. The longest study of hypoglycaemia and cognitive decline took place among participants with type 1 diabetes in the DCCT and Epidemiology of Diabetes Interventions and Complications; this found no association over a period of 18 years, but the participants had a mean age of 46 at follow-up [11]. It is possible that in young to middle-aged adults, cognitive changes are too small to detect, or that the brain is more robust to insults than in older age [31].
In our study, the modelled domain-specific cognitive decline followed expectations, suggesting that the results could be true estimates but were underpowered. Specifically, adjustment for APOE ε4 alleles weakened the hypoglycaemia estimates for memory but not executive function, while adjustment for diabetes characteristics attenuated the hypoglycaemia estimates for executive function but not memory [18, 32]. Interestingly, the association of hypoglycaemia with cognitive decline was strongest for the memory domain, although it was not statistically significant. One possibility is that worsening short-term memory may contribute to severe hypoglycaemia, mediated by difficulty in remembering to take medications or to eat. In light of the strong association with dementia, the lack of clear association with cognitive decline could be due to the mix of study participants: some with low baseline cognitive function without much decline, needing less loss to reach dementia, and others with high cognitive function but rapid decline, leading to large variability in cognitive decline and non-significant results. Future research should consider baseline cognitive function carefully in analyses of cognitive decline and dementia.
There are clear mechanisms by which severe hypoglycaemia leads to neurological damage, but it is unclear whether the physiological extremes of hypoglycaemia in animal studies apply to hypoglycaemia in type 2 diabetes. Hypoglycaemia can cause neuronal cell death either directly or via a variety of other mechanisms, including increased glutamate production, reactive oxygen species and activation of poly(ADP-ribose) polymerase [33]. In studies of insulin-induced hypoglycaemia in monkeys, blood glucose concentrations of <1.11 mmol/l were required for 5–6 h before neurological damage occurred, and this duration of hypoglycaemia is likely to be uncommon in humans [33]. The effect of repeated episodes of less severe and shorter duration hypoglycaemia on the neurological function of older adults is unknown. Our study relied on single severe episodes of hypoglycaemia, but this probably also reflects recurrent mild episodes of hypoglycaemia. Although our study provides additional evidence, it cannot prove causality in isolation.
Our findings should be interpreted in the context of certain study limitations. First, we cannot establish temporality for our cross-sectional results. Second, there may be survival bias wherein individuals with severe hypoglycaemia who attended the study visits were likely to be healthier than those who did not attend the study visit. However, in our study, the odds of prevalent dementia when comparing individuals with and without hypoglycaemia were similar whether or not participants attended the study visit. Third, similar to other epidemiological studies relying on medical insurance claims, we were only able to identify hypoglycaemic episodes that resulted in emergency medical treatment. Fourth, our analysis of brain volumes included only 12 participants with hypoglycaemia and thus should be considered preliminary. Fifth, we evaluated a number of outcomes, increasing the risk of type 1 error. Finally, we did not have enough participants with two or more hypoglycaemic episodes to look at a dose–response relationship.
There are also strengths of our analyses. First, our assessments of mild cognitive impairment and dementia were based on robust criteria using a wide range of data, and each case was reviewed by an expert dementia committee to determine the diagnosis and probably aetiology [21]. Second, we were able to adjust for likely confounders including educational attainment and APOE genotype, which affect baseline cognitive function and rate of cognitive decline, respectively.
Clinical guidelines from the ADA currently recommend annual screening for cognitive impairment among older adults with diabetes [2]. Given the high burden of cognitive impairments and poor prognosis in individuals with a history of hypoglycaemia in our study, it may be worth considering severe hypoglycaemia as a prompt to providers to reassess cognitive function and determine whether individuals’ diabetes self-management skills may be diminished.
Strategies for the prevention of hypoglycaemia among older adults are currently in development; these include risk-prediction algorithms to identify individuals at high risk of hypoglycaemia [34] and determining the best approaches to adjusting glucose-lowering medications, particularly insulin [35]. Although some health systems have implemented electronic medical record-based alerts to prompt re-evaluation of diabetes treatment in older adults, it remains to be seen whether the implementation of these strategies will reduce severe hypoglycaemic episodes [36].
In conclusion, among older adults with diabetes, those with severe hypoglycaemia have a high burden of cognitive dysfunction and are at increased risk of dementia. Careful consideration of baseline cognitive function is warranted in future analyses of hypoglycaemia and cognitive decline and dementia. Further studies are needed to determine whether interventions designed to reduce hypoglycaemia could prevent or delay cognitive decline and dementia.
Data availability
The datasets analysed during the current study are not publicly available due to the possibility that some information in these data might compromise research participants’ privacy or consent. However, data are available from the corresponding author on request.
Abbreviations
- ARIC:
-
Atherosclerosis Risk in Communities
- CDR:
-
Clinical Dementia Rating
- TICS:
-
Telephone Interview for Cognitive Status
References
Seaquist ER, Anderson J, Childs B et al (2013) Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine society. Diabetes Care 36:1384–1395
American Diabetes Association (2017) Standards of Medical Care in Diabetes -- 2017. Diabetes Care 40(Supp 1)
Warren RE, Frier BM (2005) Hypoglycemia and cognitive function. Diabetes Obes Metab 7:493–503
Kang E, Jeon S, Choi S, Song C, Yu I (2010) Diffusion MR imaging OF hypoglycemic encephalopathy. Am J Neuroradiol 31:559–564
Ma JH, Kim YJ, Yoo WJ et al (2009) MR imaging of hypoglycemic encephalopathy: lesion distribution and prognosis prediction by diffusion-weighted imaging. Neuroradiology 51:641–649
Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP Jr, Selby JV (2009) Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA 301:1565–1572
Yaffe K, Falvey CM, Hamilton N et al (2013) Association between hypoglycemia and dementia in a biracial cohort of older adults with diabetes mellitus. JAMA Intern Med 173:1300–1306
Lin CH, Sheu WHH (2013) Hypoglycaemic episodes and risk of dementia in diabetes mellitus: 7-year follow-up study. J Intern Med 273:102–110
Bruce DG, Davis WA, Casey GP et al (2009) Severe hypoglycaemia and cognitive impairment in older patients with diabetes: the Fremantle Diabetes Study. Diabetologia 52:1808–1815
Feinkohl I, Aung PP, Keller M et al (2014) Severe hypoglycemia and cognitive decline in older people with type 2 diabetes: the Edinburgh type 2 diabetes study. Diabetes Care 37:507–515
Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group (2007) Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med 356:1842–1852
National Institute of Neurological Disorders and Stroke. Dementia information page. Available from www.ninds.nih.gov/disorders/all-disorders/dementia-information-page#disorders-r1? Accessed 7 Apr 2018
Mattishent K, Loke YK (2016) Bi-directional interaction between hypoglycaemia and cognitive impairment in elderly patients treated with glucose-lowering agents: a systematic review and meta-analysis. Diabetes Obes Metab 18:135–141
Punthakee Z, Miller ME, Launer LJ et al (2012) Poor cognitive function and risk of severe hypoglycemia in type 2 diabetes: post hoc epidemiologic analysis of the ACCORD trial. Diabetes Care 35:787–793
De Galan BE, Zoungas S, Chalmers J et al (2009) Cognitive function and risks of cardiovascular disease and hypoglycaemia in patients with type 2 diabetes: the action in diabetes and vascular disease: preterax and diamicron modified release controlled evaluation (ADVANCE) trial. Diabetologia 52:2328–2336
Lee AK, Lee CJ, Huang ES, Sharrett AR (2017) Risk factors for severe hypoglycemia in black and white adults with diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care 40:1661–1667
Prinz N, Stingl J, Dapp A et al (2015) High rate of hypoglycemia in 6770 type 2 diabetes patients with comorbid dementia: a multicenter cohort study on 215,932 patients from the German/Austrian diabetes registry. Diabetes Res Clin Pract 112:73–81
Rawlings AM, Sharrett AR, Schneider ALC et al (2014) Diabetes in midlife and cognitive change over 20 years: a cohort study. Ann Intern Med 161:785–793
ARIC Investigators (1989) The Atherosclerosis Risk In Communities (ARIC) Study: design and objectives. Am J Epidemiol 129:687–702
Ginde AA, Blanc PG, Lieberman RM, Camargo CA (2008) Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord 8:4
Knopman DS, Gottesman RF, Sharrett AR et al (2016) Mild cognitive impairment and dementia prevalence: the Atherosclerosis Risk in Communities Neurocognitive Study (ARIC-NCS). Alzheimers Dement 2:1–11
Gottesman RF, Albert MS, Alonso A et al (2017) Associations between midlife vascular risk factors and 25-year incident dementia in the Atherosclerosis Risk in Communities (ARIC) Cohort. JAMA Neurol 74:1246–1254
Knopman DS, Griswold ME, Lirette ST et al (2015) Vascular imaging abnormalities and cognition: mediation by cortical volume in nondemented individuals: Atherosclerosis risk in Communities-Neurocognitive Study. Stroke 46:433–440
ARIC Investigators. ARIC Visit 5/NCS Analysis Manual. Available from www2.cscc.unc.edu/aric/sites/default/files/public/listings/V5%20NCS%20Analysis%20Manual_150901%20v1.pdf. Accessed 3 June 2017
Gross AL, Power MC, Albert MS et al (2015) Application of latent variable methods to the study of cognitive decline when tests change over time. Epidemiology 26:878–887
Georgakis MK, Dimitriou NG, Karalexi MA (2017) Albuminuria in association with cognitive function and dementia: a systematic review and meta-analysis. J Am Geriatr Soc 65:1190–1198
Helmer C, Stengel B, Metzger M et al (2011) Chronic kidney disease, cognitive decline, and incident dementia: the 3C Study. Neurology 77:2043–2051
Zhang Z, Lovato J, Battapady H et al (2014) Effect of hypoglycemia on brain structure in people with type 2 diabetes: epidemiological analysis of the ACCORD-MIND MRI Trial. Diabetes Care 37:3279–3285
Auer RN, Siesjo BK (1993) Hypoglycaemia: brain neurochemistry and neuropathology. Bailliere Clin Endocrinol Metab 7:611–625
Schneider ALC, Selvin E, Sharrett AR et al (2017) Diabetes, prediabetes, and brain volumes and subclinical cerebrovascular disease on MRI: the Atherosclerosis Risk in Communities Neurocognitive Study (ARIC-NCS). Diabetes Care 40:1514–1521
Biessels GJ, Strachan MWJ, Visseren FLJ, Kappelle LJ, Whitmer RA (2014) Dementia and cognitive decline in type 2 diabetes and prediabetic stages: towards targeted interventions. Lancet Diabetes Endocrinol 2:246–255
Wilson RS, Schneider JA, Barnes LL et al (2002) The apolipoprotein E epsilon 4 allele and decline in different cognitive systems during a 6-year period. Arch Neurol 59:1154–1160
Cryer PE (2007) Hypoglycemia, functional brain failure, and brain death. J Clin Invest 117:868–870
Karter AJ, Warton EM, Lipska KJ et al (2017) Development and validation of a tool to identify patients with type 2 diabetes at high risk of hypoglycemia-related emergency department or hospital use. JAMA Intern Med 36:3535–3542
Munshi MN, Slyne C, Segal AR, Saul N, Lyons C, Weinger K (2016) Simplification of insulin regimen in older adults and risk of hypoglycemia. JAMA Intern Med 176:1023–1025
Vimalananda VG, DeSotto K, Chen T et al (2017) A quality improvement program to reduce potential overtreatment of diabetes among veterans at high risk of hypoglycemia. Diabetes Spectr 30:211–216
Acknowledgements
The authors thank the staff and participants of the ARIC study for their important contributions.
Funding
The ARIC study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health, Department of Health and Human Services, under Contract nos. HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I and HHSN268201700004I. Neurocognitive data were collected by U01 2U01HL096812, 2U01HL096814, 2U01HL096899, 2U01HL096902 and 2U01HL096917 from the NIH (NHLBI, National Institute of Neurological Disorders and Stroke (NINDS), National Institute on Aging (NIA) and National Institute on Deafness and Other Communications Disorders (NIDCD)), with previous brain MRI examinations funded by R01-HL70825 from the NHLBI. This research was supported by NIH/NIDDK grants K24DK106414 and R01DK089174 to ES. AKL and AMR were supported by NIH/NHLBI grant T32HL007024. CJL was supported by NIH/NIDDK grant 1K23DK107921. ESH was supported by K24DK105340, R01HS018542 and P30DK092949.
Author information
Authors and Affiliations
Contributions
AKL conceived and designed the study, conducted statistical analyses and drafted the manuscript. AMR and ALG contributed to the statistical analyses and made critical revisions to the manuscript for important intellectual content. CJL, ESH, ARS, and JC contributed to the interpretation of data for the work and made critical revisions to the manuscript for important intellectual content. ES made contributions to the conception and design of the study and to the interpretation of data for the work, and made critical revisions to the manuscript for important intellectual content. All authors had final approval of the version to be published. ES is responsible for the integrity of the work as a whole.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 257 kb)
Rights and permissions
About this article
Cite this article
Lee, A.K., Rawlings, A.M., Lee, C.J. et al. Severe hypoglycaemia, mild cognitive impairment, dementia and brain volumes in older adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) cohort study. Diabetologia 61, 1956–1965 (2018). https://doi.org/10.1007/s00125-018-4668-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4668-1