Abstract
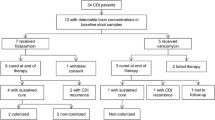
PURPOSE: Antibiotics suppress normal gut flora, allowing overgrowth of acquired or nativeClostridium difficile, with release of toxins that cause mucosal inflammation. Oral metronidazole is used to treat antibiotic-associated colitis (pseudomembranous colitis). This study was designed to determine whether oral metronidazole, as part of preoperative bowel preparation, prevents or decreases incidence of antibiotic-associated colitis after elective colonic and rectal procedures. METHODS: Eighty-two patients (40 men) were prospectively, randomly assigned to receive one of two oral antibiotic regimens before colorectal surgery. All patients underwent mechanical bowel preparation with polyethylene glycol-electrolyte lavage solution before administration of oral antibiotics. Group 1 (n=42) patients received three doses (1 g/dose) of neomycin and erythromycin. Group 2 (n=40) patients received three doses (1 g/dose) of neomycin and metronidazole. Both groups received one preoperative and three postoperative doses of intravenous cefotetan (2 g/dose). Both groups had stool samples tested forC. difficile toxin in the preoperative and postoperative periods by enzyme-linked immunoabsorbent assay or by tissue culture cytotoxicity. Patients with preoperative stool studies positive forC. difficile were excluded from the study. RESULTS: Treatment groups were not different for age, gender, or surgical procedure. Mean age ±1 standard deviation was 67.6±13.6 (range, 34–94) years in Group 1 and 62.1±13.5 (range, 35–84) years in Group 2 (P=0.069). Mean length of hospital stay ±1 standard deviation was 9.76±4.9 (range, 4–28) days for Group 1 and 8.05±2.6 (range, 3–14) days for Group 2 (P=0.053). Five patients in Group 1 (neomycin and erythromycin) and one patient in Group 2 (neomycin and metronidazole) had positive stool studies forC. difficile. Relative risk of colonization withC. difficile in Group 1 was 4.76 times that in Group 2 (95 percent confidence interval, 0.581, 39). This difference was not statistically significant (P=0.202). There were no significant differences inC. difficile colonization rates with respect to age, length of stay, or gender. CONCLUSIONS: This study suggests that there may be a clinical association between use of metronidazole preoperatively and inhibition of intestinal colonization byC. difficile in this patient population undergoing colonic and rectal surgery.
Similar content being viewed by others
References
Finney JM. Gastroenterostomy for cicatratizing ulcer of the pylorus. Bull Johns Hopkins Hosp 1893;4:53–5.
Altemeier WA, Hummel RP, Hill EO. Staphylococcal enterocolitis following antibiotic therapy. Ann Surg 1963;157:847–58.
Marr JJ, Sans MD, Tedesco FJ. Bacterial studies of Clindamycin-associated colitis. Gastroenterology 1975;69:352–8.
Fekety R, Shah AB. Diagnosis and treatment ofClostridium difficile colitis. JAMA 1993;269:71–5.
Bartlett JG, Chang TW, Gurwith M, Gorbach SL, Onderdonk AB. Antibiotic associated pseudomembranous colitis due to toxin-producing clostridia. N Engl J Med 1978;298:531–4.
Trnka YM, Lamont JT.Clostridium difficile colitis. Adv Intern Med 1984;29:85–107.
Rosen L. Antibiotic-associated colitis. Perspect Colon Rectal Surg 1991;4:205–17.
Marts BC, Longo WE, Vernava AM III, Kennedy DJ, Daniel GL, Jones I. Patterns and prognosis ofClostridium difficile colitis. Dis Colon Rectum 1994;37:837–45.
Tedesco FJ. Pseudomembranous colitis: pathogenesis and therapy. Med Clin North Am 1982;66:655–64.
Kelly CP, Pothoulakis C, LaMont JT.Clostridium difficile colitis. N Engl J Med 1994;330:257–62.
Medich DS, Lee KK, Simmons RL, Grubbs PE, Yang HC, Showalter DP. Laparotomy for fulminant pseudomembranous colitis. Arch Surg 1992;127:847–53.
Jobe BA, Grasley A, Deveney KE, Deveney CW, Sheppard BC.Clostridium difficile colitis: an increasing hospital-acquired illness. Am J Surg 1995;169:480–3.
Rudensky B, Rosner S, Sonnenblick M, van Dijk Y, Shapira E, Isaacsohn M. The prevalence and nosocomial acquisition ofClostridium difficile in elderly hospitalized patients. Postgrad Med 1993;69:45–7.
Silva J. Update on pseudo-membranous colitis. West J Med 1989;151:644–8.
McCarter MD, Abularrage C, Velasco FT, Davis JM, Daly JM. Diarrhea andClostridium difficile-associated diarrhea on a surgical service. Arch Surg 1996;131:1333–7.
Lipsett PA, Samantaray DK, Tam ML, Bartlett JG, Lillemoe KD. Pseudomembranous colitis: a surgical disease? Surgery 1994;116:491–6.
Yee J, Dixon CM, McLean AP, Meakins JL.Clostridium difficile disease in a department of surgery: the significance of prophylactic antibiotics. Arch Surg 1991;126:241–6.
Rubin MS, Bodenstein LE, Kent KC. SevereClostridium difficile colitis. Dis Colon Rectum 1995;38:350–4.
Holmes NJ.Clostridium difficile colitis. Curr Surg 1996;53:16–9
Gerding DN, Olson MM, Johnson S, Peterson LR, Lee JT Jr.Clostridium difficile diarrhea and colonization after treatment with abdominal infection regimens containing clindamycin or metronidazole. Am J Surg 1990;159:212–7.
Author information
Authors and Affiliations
Additional information
Supported, in part, by the Department of Research at St. Joseph Mercy Hospital, Ann Arbor, Michigan.
About this article
Cite this article
Cleary, R.K., Grossmann, R., Fernandez, F.B. et al. Metronidazole may inhibit intestinal colonization withClostridium difficile . Dis Colon Rectum 41, 464–467 (1998). https://doi.org/10.1007/BF02235760
Issue Date:
DOI: https://doi.org/10.1007/BF02235760